by Dr. Talia Marcheggiani, ND | Jan 17, 2018 | Addiction, Community, Healing Stories, Health, Medicine, Mental Health, Volunteering
 An interview outlining my adventures providing free naturopathic medicine to street youth at the Evergreen Yonge Street Mission health centre, originally featured in Pulse, a publication for members of the Ontario Association of Naturopathic Doctors.
An interview outlining my adventures providing free naturopathic medicine to street youth at the Evergreen Yonge Street Mission health centre, originally featured in Pulse, a publication for members of the Ontario Association of Naturopathic Doctors.
What is the Evergreen Yonge Street Mission?
On the fourth Friday of every month, I leave my Bloor West Village practice for a few hours and head down Yonge Street.
Just south of Gerard, I stop at a rather unimpressive-looking building tucked between fast-food restaurants and strip clubs, where an admittedly intimidating crowd of young people are smoking and laughing loudly, hoodies drawn.
I nod to them briefly before heading past them, through a glass-paneled doorway.
The entrance is crowded. Youth and tattooed counselors blast rap music out of large headphones. Some of them have notebooks, writing lyrics.
Beyond them is an open area where food is being served; more young people sit at round tables, finishing hot catered lunches, or drinking coffee. A few are involved in some community project or other, conspiring excitedly in groups. Everyone seems to be embracing a perplexing combination of busyness and inertia.
I smile at them and rush downstairs to the basement, past the career centre to the unglamorous health centre where my tiny office is located.
The Evergreen Yonge Street Mission (YSM) is a drop-in centre for street-involved youth aged 18 to 24 that offers afternoon programming, including a hot lunch, career services, daycare, community-based art projects, and drop-in healthcare centre.
The health centre is run by nurse practitioners and staffed by volunteer health professionals: adolescent health specialists, family doctors, Sick Kids residents, dentists, hygienists, acupuncturists, chiropractors, physiotherapists, social workers, psychiatrists and, of course, two naturopathic doctors, Dr. Leslie Solomonian, and myself.
Youth drop in during health centre hours and sign up for 30-minute appointments with the practitioner of their choice.
How did you start working with the Mission?
I first visited the Evergreen YSM for a launch party for the second issue of Street Voices, a magazine for and by street-involved youth. A friend of mine had volunteered to do most of the graphic design and illustration work for the issue and brought me along.
At the party, while eating tiny sandwiches, I noticed a message board advertising YSM services. Naturopathic medicine was listed under health services provided at the centre. I took down the number of the health centre, and gave them a call the following week.
By February 2015, I was volunteering two Fridays a month.
Why did you decide to get involved with the Mission?
I came across Evergreen at the beginning of my naturopathic career. I’d just obtained my license in 2014, and was looking for a way to balance the cost of living and running a practice with providing access to naturopathic services.
Naturopathic medical services have the potential to be very cost-effective; our profession was built on the foundations of clean air, food, and water as vehicles for healing. Nature cure, lifestyle therapies, and in-house treatments like acupuncture can all be very inexpensive to administer.
Unfortunately, the cost of education, licensing fees, and practice overhead all conspire to bring up the cost of naturopathic services, making it difficult for those without third-party insurance coverage to afford them.
When I first started my practice, I tried to find various solutions to this problem. I dabbled in sliding scales but quickly started to notice burnout and resentment polluting my therapeutic relationships. Separating cost, value and worth, while accurately assessing need, complicated things for me—I found it very difficult to lower my rates while still recognizing the value I was offering.
Dispensing with sliding scales at my main practice while offering free services to a marginalized population felt like a satisfactory compromise: I could build my practice, pay for my groceries, and give back, while maintaining clear boundaries.
What type of naturopathic care do you provide at the YSM?
There are a few ways that my YSM practice differs from my practice in Bloor West Village.
Firstly, visits are shorter. The YSM suggests keeping visits to 30 minutes to serve as many patients as possible. Keeping visits short is a challenge for me, considering appointments in my Bloor West practice run 60 to 90 minutes.
Secondly, therapeutic options are limited. Patients don’t have the cash to buy supplements. Making significant dietary changes is impossible for most to tackle. Therefore, I try to offer therapies in the clinic: acupuncture, B12 shots, homeopathic remedies, and counseling, to reduce the work between appointments.
Sometimes we have supplements to dispense—Cytomatrix generously donated last year. At times we’ve been able to offer things like magnesium, vitamin D, iron, immune support, adaptogens, and sample packs of various probiotics.
Treatment plans often require a bit of innovation. For example, I teach patients how to use the probiotic samples to make coconut yogurt using canned coconut milk from food banks. We talk about how to follow an anti-inflammatory diet while eating at a shelter.
Thirdly, there are many obstacles that prevent patients from attending appointments in the first place. I try to treat each visit as a stand-alone encounter—a new patient I see at Evergreen may never come back. This means I focus on stress-reduction and providing as much benefit as possible in the 30-minute session.
What does a typical visit look like?
Visits can differ greatly depending on the particular needs of the patients I see.
Sometimes new patients come in asking specifically for trigger-point release acupuncture.
One patient came in with her friend so they could Snapchat their first acupuncture session amidst violent giggling.
Some patients come to talk about their struggles and share their stories.
Sometimes patients come in to read me their rap or poetry.
Sometimes patients just come in to sleep—the flimsy chiropractic table we use serving as a quiet, 30-minute refuge from the street. Sometimes we do a mindfulness practice. Other times we say very little, or nothing at all.
Others come for full intakes, with complicated psychiatric cases, or PCOS, or chronic diarrhea. I try to hand out any supplements that might be useful, and to give practical recommendations.
Sometimes patients with part-time jobs have a little money that they can spend on things like St. John’s Wort, magnesium, or vitex.
I have to be extremely economical with my therapies, which I feel is a helpful skill to have as an ND in general—I learn what simple treatments have the biggest impact on certain conditions. This helps me resist the temptation of loading patients down with complicated, expensive treatment plans.
What are some strategies for working with this population?
When working with street-involved youth, I’ve found it helpful to humbly take a step back and listening first before jumping in with solutions.
A de-centred practitioner posture can be particularly helpful in a population experiencing homelessness, violence, complex trauma, addiction, teen pregnancy, abuse, conflict with authority, and severe psychiatric illnesses, among other complex challenges—it’s not always clear what to do, what might best help the individual in front of me, and deferring to their experience is often the wisest first step.
De-centring positions the clinician as a guide, facilitator, or someone of service to the patient. This means that I offer my tools: an ear, acupuncture, vitamin D, or a sanctuary of silence, and let my patients choose whatever they want for their 30-minute appointment.
Another helpful skill is being interested in all my patients’ stories, even the ones that aren’t being told about them.
In Narrative Therapy this is called “double-listening”. Accompanying every story of illness, addiction, label of mental illness, or history of trauma, is a parallel story of strength, courage, generosity, and overcoming tremendous obstacles.
I can be a witness to the alternative stories, which are often begging to be told.
Sometimes addiction, self-harm, or other seemingly “destructive” behaviours, may be hidden coping mechanisms that serve as powerful lifelines for survival. Listening between the lines can highlight certain skills and strengths of those who suffer.
A mentor of mine, when faced with an “angry” client, always asks, “What are you protesting?” With that simple reframing question she often uncovers previously hidden stories of belief in fairness, advocacy for justice, courage, and resilience.
Patients tell me about their issues, but also about their beloved pets, how they wish they could be a better father to their children than their fathers were to them, family loyalty in the face of abuse, their dreams for the future, the steps they’ve taken to confront a friend’s addiction, their hopes for a healthier romantic relationship, and many other stories. These narratives depict the complex facets of their identities: street-youth, yes, but also loving parents, friends, budding entrepreneurs, and gifted artists.
One patient who’d recently been diagnosed with schizophrenia told me about the voices in her head. I asked her what the voices said when they spoke to her.
She looked at me, stunned.
“No one’s ever asked me that before.”
This question led us to an important discussion about how she’d turned to writing poetry and her faith to help her stop using methamphetamine. The voices, while often unpleasant, were keeping her sober in their own complex way, she realized.
Through paying careful attention to these stories, patients can reframe and foster preferred identities.
Do you have any stories in particular?
There are many stories of resilience at Evergreen. I have had the opportunity to watch one of my patients transform his life over the past couple of years.
With a criminal record for assault, anger management issues, difficulty holding a job, a mild learning disability, and a history of complex trauma, this individual picked up the pieces of himself, slowly.
The last time I saw him he had completed a yoga teacher training, begun classes at U of T, and was getting ready to move out of the shelter he’d been living in, into his own small apartment.
Through his own remarkable resilience, and some support he was able to receive at Evergreen, he was able to get himself onto an amazing and exciting path. Seeing potential realized is an amazing experience.
Like tending to a garden of souls; you might help plant seeds, or tend to the soil in very simple, minimal ways, and yet amazing things bloom.
What benefits has this work brought to you as an ND?
I believe working with diverse populations enriches practitioner experience. It reminds me to stay open to experiences, personalities, viewpoints, and unique patient histories.
Listening helps me calm the “righting reflex”: the reflex to jump quickly to a solution in order to soothe my own discomfort of sitting with the agony of uncertainty.
I notice in my own practice when I take a more de-centred stance, roll with resistance, and really pay attention to my patient’s preferences and intuition, I am better able to assist them in healing. Not only does letting the patient take the lead result in better outcomes, it also reduces the burden of (impossible) responsibility by shifting the locus of control, preventing burnout.
I struggle with this in my own practice at times; I frequently feel pressure to prove myself. Working at Evergreen helps remind me that we can’t necessarily help everyone for everything in every circumstance.
All of our patients surpass incredible external and internal obstacles to arrive at our offices and face still more difficulties between visits. Trying to recognize and work with these struggles as best we can, taking small but meaningful steps in and between visits, and acknowledging that sometimes it’s about planting seeds of change, which may take months or even years before they’re ready to bloom.
No matter how impatient I might be feeling with a patient’s progress, I try to remember that steps are constantly being taken in the direction of healing.
What are some challenges?
Like any novice practitioner I am accompanied by two familiar acquaintances: self-doubt and second-guessing. These two friends take their place beside me both in my Bloor West practice and at Evergreen.
Celebrating small victories has been important, but so has staying humble. As the mantra goes: the patient heals them-self.
I try to remember this when I’m either feeling too self-congratulatory or too down on myself.
Funding for supplements, energy, avoiding burnout, and being productive with time, are all familiar challenges I also routinely experience.
I always wish I had more time, better and more exciting remedies to dispense, and more energy to really immerse myself in the dedication community work demands.
I try to take the stance of simply being of service while trying to remain free of expectation.
How can other NDs wanting to do similar work get involved?
If you’re interested in working with marginalized populations, the first thing to do is get in touch with local shelters, such as Covenant House or Eva’s Place.
Many shelters offer satellite health services, such as massage therapy. Perhaps start by offering acupuncture, or other forms of bodywork. Acupuncture is an accessible modality that is cost-efficient and fits well with a drop-in model—patients derive benefit from the session and aren’t expected to make significant lifestyle changes or purchase supplements, both of which may be impossible.
Often stress-relief is the first primary goal of care, as is creating a safe space and nurturing trust between the clinician and community.
If you’re willing to offer your services for free there are many populations in Toronto and the GTA that could benefit greatly from naturopathic care.
How can we help?
The YSM is currently accepting donations to help build their new location, and complete their new health centre. Visit https://www.ysm.ca/donate/ to make a one-time, or monthly donation, and help a great cause.
If you would like to donate supplements, acupuncture needles, homeopathic, or herbal remedies please contact me!

by Dr. Talia Marcheggiani, ND | Aug 30, 2015 | Acupuncture, Addiction, Community, Healing Stories, Health, Human Rights, Listening, Medicine, Mental Health, Motivation, Philosophy, Politics, Psychology, Volunteering
 I was recently told that a benefactor would contact me about the work I’ve been doing for the Evergreen Yonge Street Mission in Toronto—I provide naturopathic services to street-involved youth twice a month in the drop-in health clinic. There is a natural health company that might be interested in sponsoring some of the naturopathic services. However, in order to understand where their money is going, they want to hear some success stories before they consider if and how much to donate. Are the services working? They want to know. Since I, more than anyone, appreciate the power of a story and, since I’m trying to raise some money to expand the services I provide myself, I thought I’d tell one. Names and details have been changed.
I was recently told that a benefactor would contact me about the work I’ve been doing for the Evergreen Yonge Street Mission in Toronto—I provide naturopathic services to street-involved youth twice a month in the drop-in health clinic. There is a natural health company that might be interested in sponsoring some of the naturopathic services. However, in order to understand where their money is going, they want to hear some success stories before they consider if and how much to donate. Are the services working? They want to know. Since I, more than anyone, appreciate the power of a story and, since I’m trying to raise some money to expand the services I provide myself, I thought I’d tell one. Names and details have been changed.
—
A shift at the mission lasts a few hours. Youth sign up for the adolescent medicine specialist and her Sick Kid’s Hospital resident, dental work or me, the naturopath, represented under the heading “naturopathic medicine/acupuncture”. There is no money for supplements—and supplements can be expensive—and the youth I treat don’t have money to buy food let alone a bottle of melatonin. So I do acupuncture.
Eduardo was waiting when it I called him. He was lying face up on the bench in the waiting area, looking at a pamphlet on “dope addiction”. He was wearing sunglasses. When he came into the visit, he didn’t take them off, despite the low-level lighting of the treatment room I occupy. It felt strange to talk to someone’s dark glasses, not making eye contact with them as we spoke. I wondered vaguely if I should tell him to take off the glasses, and then left it alone—his comfort as the patient should take priority over mine. Why challenge his autonomy and further push the power imbalance by telling him to do something that was not fully necessary? I worked around the glasses, moving them aside slightly in order to needle the acupuncture point yin tang, located between the eyebrows. The glasses stayed on. So be it.
Eduardo and I spoke Spanish, as his English wasn’t strong. He spoke of feeling shaky, showing me his tremoring hand to prove it. When did the shakiness start? I inquired. When I overdosed on crack, he explained. Well, that would do it, I thought to myself, although you can imagine my clinical experience with crack overdose was limited—there aren’t that many crack overdoses in Bloor West Village.
As it turned out, Eduardo had a significant dependence on marijuana, smoking 7 grams a day while in his home country. When he bought pot on the streets in Toronto, however, he found one deal laced with crack. He ended up in the hospital after smoking it. Another time, his weed was laced with meth.
He held his hand up. I watched it shake. He told me his whole body felt shaky. This would be exacerbated further if he stopped smoking marijuana, he assured me. Had he ever stopped before? I asked. Yes, he said. Why did he stop? I asked him, taking a de-centred approach while staying curious about preferred ways of being. In this case I suspected he preferred to be sober—after all, something had made him stop.
The cost, he explained.
Ah, that, I thought. Well, it makes sense.
Any other reason? I asked him.
He explained that his family didn’t approve. I asked him why. What might they think of marijuana? What did they see him do when he was high that led to their disapproval. Eduardo couldn’t answer. He changed the subject and explained he’d gone back to weed after quitting it that time because it helped him sleep. Since the episode with the crack overdose, though, sleep was difficult. That’s why he was here: to get acupuncture to help with sleep.
Eduardo spoke in a low voice, often responding with a word or two. Despite the glasses shielding his eyes, he kept his gaze on the floor. When I had him lie on the treatment table, I encouraged him to close his eyes and rest while the acupuncture worked.
After a few minutes, I removed the needles. He thanked me shyly and left. Like many of the people I treat, I figured the odds were high I’d never see him again.
—
I was surprised, then, that a month later, I saw him in the waiting area again.
The visit went pretty much the same way as the first with one key difference. The second time he came in, Eduardo removed his glasses, meeting my eyes for the first time.
I was touched.
His sleep was still bad. His mood was still low. He hadn’t smoked crack for a while. He was living in a shelter; his family had kicked him out because of his addiction to marijuana. He implied great trauma in his home country, however he didn’t say much more about it. He mentioned regretting that his English was poor—it had been traumatic to come to Canada.
He told me he was applying for medical marijuana. It would be a safer way to smoke, he told me.
He was practicing harm reduction on himself. I asked him if he considered this “taking steps.” He nodded. I asked him about any other steps he’d been considering. He mentioned swimming. Swimming had been a passion of his in his home country. I got more details about his goals: how often did he want to swim? Where? He decided that 3-5 times a week at the local pool would be ideal. I asked him what he’d first have to do to make that happen. Check the pool times, he answered.
I asked him if he’d ever considered quitting marijuana. He said no, he needed it to sleep and to manage his anxiety. But, you know, it was expensive. And, of course, he repeated, his parents had an issue with it. That was a problem for him. I asked him why it was a problem.
It’s a problem… he repeated. He said nothing more.
We did more acupuncture. He went on his way.
—
Two weeks later, Eduardo came to see me again. He took his glasses off as soon as he saw me.
He reported his sleep was better. He had been swimming 3 times a week at the local pool. He hadn’t smoked crack in a month. He’d stopped marijuana the last time he saw me. He hadn’t smoked for two weeks. He showed me his hand. It wasn’t shaking.
Do you think these are positive developments? I asked him.
He shrugged nonchalantly but failed to disguise the smile that tugged at the corners of his mouth. He looked down.
I put in some acupuncture needles and asked him what his next steps might be. He answered that he thought he might call his old boss back and get back to work. Then he wanted to save money so he could move out of the shelter he was in.
He then started to talk a little bit about his brother who was killed in his home country and his friends who’d betrayed him to another gang resulting in him having to flee for his life. He talked about receiving premonitions in his dreams. This made sleep difficult, but it had also caused him to act and avoid harm—he’d learned from a dream that his friends were untrustworthy. We wondered together if this was more than a source of anxiety, but a special skill that kept him safe. Maybe he wouldn’t have to be vigilant if important warnings came to him in his dreams. I wondered if marijuana, along with helping hims sleep had hindered that gift. He thought about that for a while.
When he left he asked me how many more acupuncture treatments he might need. I told him to come in as often as he liked but 8-10 was a good starting point.
Ok, he said, it’s been 3 so far.
Right, I said. It’s been 3.
Ok, he said. See you in two weeks.
He put his glasses back on and walked out into the chaos of Yonge Street. There was a street festival going on.
—
At one point in my time spent with Eduardo, one of the staff at the mission inquired about his mental capacities. Apparently the psychiatrist he’d been working with was considering a diagnosis of mental retardation or severe learning disability–it was taking him so long to learn English and he was often slow to answer questions.
No disrespect to psychiatry: the more I work with mental health, the more respect I have for the utility, albeit limited, of psychiatric assessments and medications. For many people, and when applied delicately and sensitively, these things add powerful meaning and serve as important life savers. However, I want to emphasize the importance of lowering practitioner power, understanding the challenges another person may face in their life and respecting the autonomy, decision-making power and special skills of the individual who seeks health care. In addition, rather than looking for the problem in the person, what success stories are they bringing forth? What goals have been set and what steps have been taken already?
I often comment that the stories I hear and the conversations I have in the work I do are not the least bit depressing. Sure, the youth have dark, complicated, often horrific pasts. However, every individual is a collection of hopes, dreams, goals and personal strengths and abilities. Every person that comes to see me wants something more for themselves and has already exercised an ability to move closer to their preferred ways of being in the world, showing me the incredible capacity for human strength and endurance. The only difference, between the perspective I get to enjoy and the one seen by other health professionals, however, is that I look for stories of strength. Because strength is always there, waiting for a thoughtful question to bring it into the light.
To contribute to the Yonge Street Mission naturopathic services and for more information on the campaign, please click here. Donations are made in USD.

by Dr. Talia Marcheggiani, ND | Jul 20, 2015 | Art Therapy, Community, Creativity, Docere, Education, Emotions, Empathy, Finding yourself, Healing Stories, Health, Medicine, Mental Health, Mind Body Medicine, Mindfulness, Narrative Therapy, Philosophy, Politics, Psychology, Relationships, Self-reflection, Treating the Cause, Volunteering
 As a child, I was obsessed with stories. I wrote and digested stories from various genres and mediums. I created characters, illustrating them, giving them clothes and names and friends and lives. I threw them into narratives: long stories, short stories, hypothetical stories that never got written. Stories are about selecting certain events and connecting them in time and sequence to create meaning. In naturopathic medicine I found a career in which I could bear witness to people’s stories. In narrative therapy I have found a way to heal people through helping them write their life stories.
As a child, I was obsessed with stories. I wrote and digested stories from various genres and mediums. I created characters, illustrating them, giving them clothes and names and friends and lives. I threw them into narratives: long stories, short stories, hypothetical stories that never got written. Stories are about selecting certain events and connecting them in time and sequence to create meaning. In naturopathic medicine I found a career in which I could bear witness to people’s stories. In narrative therapy I have found a way to heal people through helping them write their life stories.
We humans create stories by editing. We edit out events that seem insignificant to the formation of our identity. We emphasize certain events or thoughts that seem more meaningful. Sometimes our stories have happy endings. Sometimes our stories form tragedies. The stories we create shape how we see ourselves and what we imagine to be our possibilities for the future. They influence the decisions we make and the actions we take.
We use stories to understand other people, to feel empathy for ourselves and for others. Is there empathy outside of stories?
I was seeing R, a patient of mine at the Yonge Street Mission. Like my other patients at the mission health clinic, R was a young male who was street involved. He had come to see me for acupuncture, to help him relax. When I asked him what brought him in to see me on this particular day, his answer surprised me in its clarity and self-reflection. “I have a lot of anger,” He said, keeping his sunglasses on in the visit, something I didn’t bother to challenge.
R spoke of an unstoppable rage that would appear in his interactions with other people. Very often it would result in him taking violent action. A lot of the time that action was against others. This anger, according to him, got him in trouble with the law. He was scared by it—he didn’t really want to hurt others, but this anger felt like something that was escaping his control.
We chatted for a bit and I put in some acupuncture needles to “calm the mind” (because, by implication, his mind was not currently calm). After the treatment, R left a little lighter with a mind that was supposedly a little calmer. The treatment worked. I attributed this to the fact that he’d been able to get some things off his chest and relax in a safe space free of judgment. I congratulated myself while at the same time lamented the sad fact that R was leaving my safe space and re-entering the street, where he’d no doubt go back to floundering in a sea of crime, poverty and social injustice. I sighed and shrugged, feeling powerless—this was a fact beyond my control, there wasn’t anything I could do about it.
The clinic manager, a nurse practitioner, once told me, “Of course they’re angry. These kids have a lot to be angry at.” I understood theoretically that social context mattered, but only in the sense that it posed an obstacle to proper healing. It is hard to treat stress, diabetes, anxiety and depression when the root causes or complicating factors are joblessness, homelessness and various traumatic experiences. A lot of the time I feel like I’m bailing water with a teaspoon to save a sinking ship; my efforts to help are fruitless. This is unfortunate because I believe in empowering my patients. How can I empower others if I myself feel powerless?
I took a Narrative Therapy intensive workshop last week. In this workshop we learn many techniques for empowering people and healing them via the formation of new identities through storytelling. In order to do this, narrative therapy extricates the problem from the person: the person is not the problem, the problem is the problem. Through separating problems from people, we are giving our patients the freedom to respond to or resolve their problems in ways that are empowering.
Naturopathic doctors approach conditions like diabetes from a life-style perspective; change your lifestyle and you can change your health! However, when we fail to separate the patient from the diabetes, we fail to examine the greater societal context that diabetes exists in. For one thing, our culture emphasizes stress, overwork and inactivity. The majority of food options we are given don’t nourish our health. Healthy foods cost more; we need to work more and experience more stress in order to afford them. We are often lied to when it comes to what is healthy and what is not—food marketing “healthwashes” the food choices we make. We do have some agency over our health in preventing conditions like diabetes, it’s true, but our health problems are often created within the context in which we live. Once we externalize diabetes from the person who experiences it, we can begin to distance our identities from the problem and work on it in creative and self-affirming ways.
Michael White, one of the founders of Narrative Therapy says,
If the person is the problem there is very little that can be done outside of taking action that is self-destructive.
Many people who seek healthcare believe that their health problems are a failure of their bodies to be healthy—they are in fact the problem. Naturopathic medicine, which aims to empower people by pointing out they can take action over their health, can further disempower people when we emphasize action and solutions that aim at treating the problems within our patients—we unwittingly perpetuate the idea that our solutions are fixing a “broken” person and, even worse, that we hold the answer to that fix. If we fail to separate our patients from their health conditions, our patients come to believe that their problems are internal to the self—that they or others are in fact, the problem. Failure to follow their doctor’s advice and heal then becomes a failure of the self. This belief only further buries them in the problems they are attempting to resolve. However, when health conditions are externalized, the condition ceases to represent the truth about the patient’s identity and options for healing suddenly show themselves.
While R got benefit from our visit, the benefit was temporary—R was still his problem. He left the visit still feeling like an angry and violent person. If I had succeeded in temporarily relieving R of his problem, it was only because I had acted. At best, R was dependent on me. At worst, I’d done nothing, or, even worse, had perpetuated the idea that there was something wrong with him and that he needed fixing.
These kids have a lot to be angry at,
my supervisor had said.
R was angry. But what was he angry at? Since I hadn’t really asked him, at this time I can only guess. The possibilities for imagining answers, however, are plentiful. R and his family had recently immigrated from Palestine, a land ravaged by war, occupation and racial tension. R was street-involved, living in poverty in an otherwise affluent country like Canada. I wasn’t sure of his specific relationship to poverty, because I hadn’t inquired, but throughout my time at the mission I’d been exposed to other narratives that may have intertwined with R’s personal storyline. These narratives included themes of addiction, abortion, hunger, violence, trauma and abandonment, among other tragic experiences. If his story in any way resembled those of the other youth who I see at the mission, it is fair to say that R had probably experienced a fair amount of injustice in his young life—he certainly had things to be angry at. I wonder if R’s anger wasn’t simply anger, but an act of resistance against injustice against him and others in his life: an act of protest.
“Why are you angry?” I could have asked him. Or, even better, “What are you protesting?”
That simple question might have opened our conversation up to stories of empowerment, personal agency, skills and knowledge. I might have learned of the things he held precious. We might have discussed themes of family, community and cultural narratives that could have developed into beautiful story-lines that were otherwise existing unnoticed.
Because our lives consist of an infinite number of events happening moment to moment, the potential for story creation is endless. However, it is an unfortunate reality that many of us tell the same single story of our lives. Oftentimes the dominant stories we make of our lives represent a problem we have. In my practice I hear many problem stories: stories of anxiety, depression, infertility, diabetes, weight gain, fatigue and so on. However, within these stories there exist clues to undeveloped stories, or subordinate stories, that can alter the way we see ourselves. The subordinate stories of our lives consist of values, skills, knowledge, strength and the things that we hold dear. When we thicken these stories, we can change how we see ourselves and others. We can open ourselves up to greater possibilities, greater personal agency and a preferred future in which we embrace preferred ways of being in the world.
I never asked R why the anger scared him, but asking might have provided clues to subordinate stories about what he held precious. Why did he not want to hurt others? What was important about keeping others safe? What other things was he living for? What things did he hope for in his own life and the lives of others? Enriching those stories might have changed the way he was currently seeing himself—an angry, violent youth with a temper problem—to a loving, caring individual who was protesting societal injustice. We might have talked about the times he’d felt anger but not acted violently (he’d briefly mentioned turning to soccer instead) or what his dreams were for the future. We might have talked about the values he’d been taught—why did he think that violence was wrong? Who taught him that? What would that person say to him right now, or during the times when his anger was threatening to take hold?
Our visit might have been powerful. It might have opened R up to a future of behaving in the way he preferred. It might have been life-changing.
It definitely would have been life-affirming.
Very often in the work we do, we unintentionally affirm people’s problems, rather than their lives.
One of the course participants during my week-long workshop summed up the definition of narrative therapy in one sentence,
Narrative therapy is therapy that is life-affirming.
And there is something very healing in a life affirmed.
More:
The Narrative Therapy Centre: http://www.narrativetherapycentre.com/
The Dulwich Centre: http://dulwichcentre.com.au/
Book: Maps of Narrative Practice by Michael White
by Dr. Talia Marcheggiani, ND | Jan 3, 2015 | Gratitude, Health, Holidays, Medicine, Mindfulness, NPLEX, Professional Development, Relationships, Volunteering
2014 has been a year of beginnings and endings. I ended two major relationships: one with the school I went to for 4 years and another with a long-term boyfriend, and began two new ones: I embarked on my own career as a naturopathic doctor and started a new relationship. The past year for me represents the tail end of several important life-cycles and the promise of exciting new beginnings.
It was the year I turned 28, starting a new 7-year karmic cycle. I broke up with my now ex-boyfriend of 5 years and finished my studies at the Canadian College of Naturopathic Medicine. I dedicated a large portion of my time to social activities, self-expansion and personal growth. I got out into the world and made new friends while strengthening old friendships. I became a little more daring and a lot more open. These changes helped groom me into a better doctor.
I spent the summer working, dating and studying for NPLEX II. I embraced new opportunities and made many new friends with co-workers, ex-classmates and complete strangers. I became more artistic.
I went to India in August and September after finishing NPLEX II. After 4 years of constantly doing, it felt wonderful to relax into the chaos of India and become an observer for a month. Simply being felt foreign and very uncomfortable at times, but also balancing. I relished the long train rides, the heat and the variety of cultures, smells and colours – especially the food. India contains a furious energy about it. It was a wonderful experience and a brilliant way to open myself up further to new experiences while exploring a different corner of the world.
When I arrived home from India I was ecstatic to find that I had passed NPLEX II and my Ontario board exams. I applied for my naturopathic licence and began looking for clinic spaces. When I met Heather Osler at the Bloor West Homeopathic & Wellness Clinic, I immediately knew that the space was an excellent fit. So far, I’ve been right. The calming, healing energy of the space and the wonderful staff have been amazing. I have been blessed with a practice that has been slowly and steadily building from my first week. I am grateful for the wonderful patients that have booked with me in 2014. I have learned a lot from them and have had the opportunity to help them feel better, something that I love to do.
2015 brings with it the promise of more successes in private practice as I grow my existing patient base and eventually add more practice days to my week. I look forward to connecting with my ex-classmates and new colleagues, to giving talks and writing blogs and connecting with the community. I will be taking a course in Motivational Interviewing (MI) at OISE at the University of Toronto this January and February. I also hope to take more courses in psychological methods to strengthen my ability to treat mental health conditions; I plan to find ways to bring my love for art and writing to the therapeutic experience.
I have the opportunity to volunteer 1-2 days a month at the Yonge Street Mission health clinic and am looking forward to spreading naturopathic medicine to the community, a passion of mine. Between my private practice and volunteer work, I hope to quickly expand the number of people I help with naturopathic medicine.
2015 will bring with it creativity, in the form of exciting new writing projects and an effort on my part to make time for painting and consuming art.
I hope 2015 will be a year of love, bringing with it more fulfilling relationships and the opportunity to strengthen my existing ones with friends, my significant other, my family and, of course, my Colombian yorkie, Coco. I learn so much from my relationships and they remain the most important part of my life. They encourage me to grow and continue to challenge me to become a better person, writer and doctor. I hope to find mentors both inside and outside my profession that challenge me to continue to grow and provide me with needed guidance on my journey.
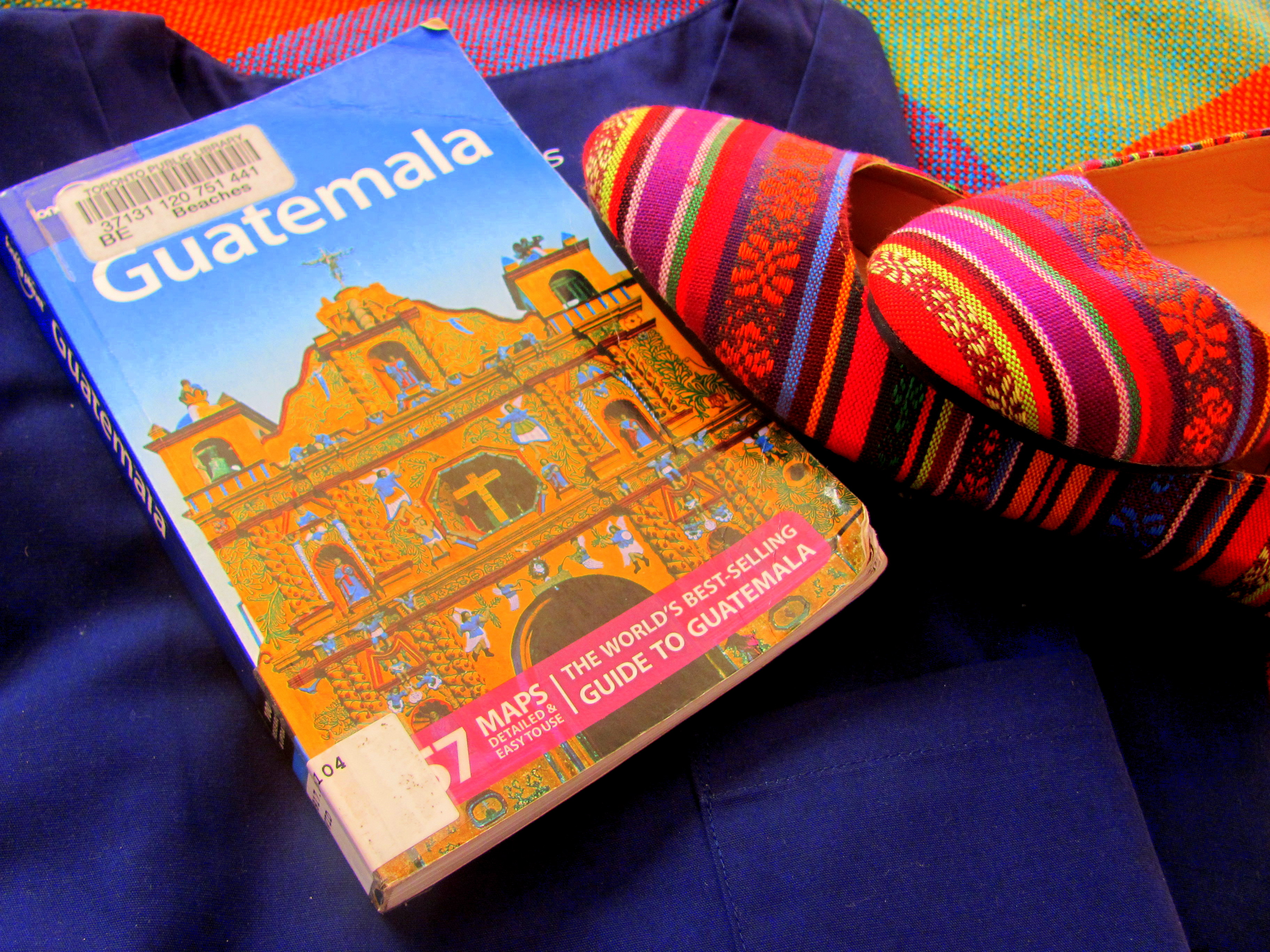
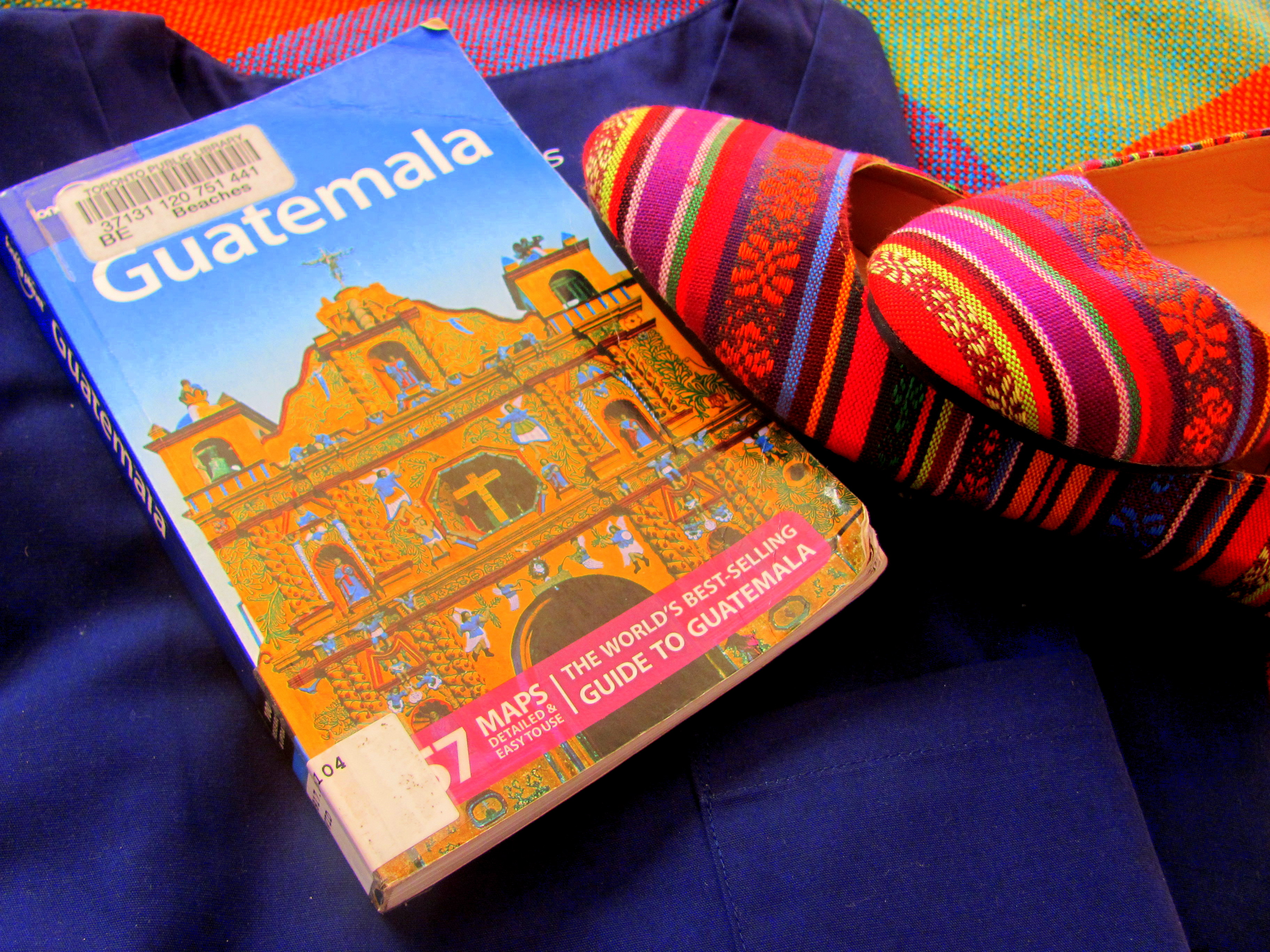
I plan to travel in 2015, to Puerto Rico, to visit the home of a dear friend and his growing family and back to Guatemala, to see my best friend in her tiny, bohemian village. I would also love to do a silent meditation retreat this year, finding more centring and balance.
I also know that 2015 will be about my own personal health. I have resolved to cut out sugar, drink more water and dedicate myself to becoming physically fitter by engaging in more yoga and strength training. I also resolve to strengthen my mindfulness practice and meditate more regularly, which I believe will help me become more conscious and present, both as a human and as a healthcare practitioner.
Most of all, I hope that 2015 will be about gratitude. As I become older, time seems to pass all the more quickly and I find this to be an alarmingly unpleasant realization. As a lifelong student and now a professional running her own business, I often find myself consumed by future goals, wants and needs, which interferes with my ability to live in the present moment, be reflective of and grateful for all the blessings I have been given in my life and currently enjoy. Dedicating myself to counting these blessings helps to anchor me to the present moment and feel happier with the wonderful life I’ve been given and the wonderful people who surround me.
2014 was an amazing year of transformation and growth. While Back to the Future II promised us a 2015 of flying cars and 80’s-style sneakers that automatically lace themselves, I believe the real 2015 will be an even better year filled with strength, opportunities for further growth and development and love. I hope to build more confidence and wisdom this year, develop more confidence in myself and add more stability to my life. 2015 will be about building strength and foundation.
I wish all of you the best this 2015. What are your reflections, hopes and resolutions for the coming year?

by Dr. Talia Marcheggiani, ND | Feb 19, 2014 | Community, Guatemala, Healing Stories, Health, Volunteering, Volunteering Abroad, Writing

We take a chicken bus to the hospital in Sololá, Guatemala. The emergency room is simple: 5 beds in a row sheltered by curtains. The sanitation conditions are questionable. There are no respirators (patients are bagged manually, all through the night) or fancy medical equipment. The emergency room is a bustling gathering place for the daily misfortunes of any of the 500,000 residents of Lago Atitlán.
My classmates and I, fresh from the airport, are dressed in navy blue scrubs, shiny and new from Walmart. I have a stethoscope around my neck: a Littman Cardio III. I’d guess that it’s the most expensive stethoscope in the hospital. It’s also auscultated the least amount of hearts; I’d be willing to bet that too.
(more…)
by Dr. Talia Marcheggiani, ND | Feb 13, 2013 | Canadian College of Naturopathic Medicine, Community, Culture, Travel, Volunteering, Volunteering Abroad
My scrubs, stethoscope and 50 pounds of supplements to donate to the Guatemalan clinic are packed and I’m ready to go! Today I’m off for my medical brigade to Guatemala with Naturopathic Medicine for Global Health (NMGH) where a group of students from the Canadian College of Naturopathic Medicine and I will be seeing patients in a free clinic outside of Panajachel that caters to the Mayan community. I’m so excited and grateful to have received this amazing opportunity. Before I leave I want to send a huge THANK YOU to everyone who donated to my cause! I’ll be back on February 24th, the day after my birthday, with (hopefully) some amazing stories and insights from my trip to share. See you all soon!

by Dr. Talia Marcheggiani, ND | Nov 30, 2012 | Canadian College of Naturopathic Medicine, Community, Guatemala, South America, Travel, Travel Stories, Volunteering, Volunteering Abroad

So, in February of 2013 I will be packing up my medical equipment and heading to Panajachel, Guatemala to embark on my first ever medical brigade with Naturopaths Without Borders (NWB) and Naturopathic Medicine for Global Health (NMGH)!
(more…)

by Dr. Talia Marcheggiani, ND | Mar 8, 2012 | Art, Balance, Colombia, Culture, Empathy, Family, Healing Stories, Listening, Love, Naturopathic Philosophy, NGOs, Photography, Psychology, South America, Travel, Travel Stories, Volunteering, Volunteering Abroad
 As mentioned before, naturopaths are not necessarily defined by our toolbox of modalities. What, then, does define us as a profession? As we witness a rise in the demand for complementary and alternative medicine, and with it, the rise in something called the “Holistic Medical Doctor”, what sets naturopathic doctors apart?
As mentioned before, naturopaths are not necessarily defined by our toolbox of modalities. What, then, does define us as a profession? As we witness a rise in the demand for complementary and alternative medicine, and with it, the rise in something called the “Holistic Medical Doctor”, what sets naturopathic doctors apart?
(more…)

 An interview outlining my adventures providing free naturopathic medicine to street youth at the Evergreen Yonge Street Mission health centre, originally featured in Pulse, a publication for members of the Ontario Association of Naturopathic Doctors.
An interview outlining my adventures providing free naturopathic medicine to street youth at the Evergreen Yonge Street Mission health centre, originally featured in Pulse, a publication for members of the Ontario Association of Naturopathic Doctors.