by Dr. Talia Marcheggiani, ND | Jan 15, 2022 | Allergies, Anxiety, Autoimmune, Depression, Detoxification, Digestion, Elimination Diet, Food, Food Sensitivities, Gut Microbiome, Leaky Gut, Nature, Nutrition, Preventive Medicine, Science
G.K. Chesterton described a scenario like this:
“There exists in such a case a certain institution or law; let us say, for the sake of simplicity, a fence or gate erected across a road. The more modern type of reformer goes gaily up to it and says, “I don’t see the use of this; let us clear it away.” To which the more intelligent type of reformer will do well to answer: “If you don’t see the use of it, I certainly won’t let you clear it away. Go away and think. Then, when you can come back and tell me that you do see the use of it, I may allow you to destroy it.”
In other words, beware of tearing down structures until you fully understand their benefit.
Chesterton’s Fence can also be thought of as the Precautionary Principle. Not following this principle led to scientific practices like frontal lobotomies or removing the entire large intestine because doctors didn’t understand the benefits of these structures or the consequences of removing them.
A narrow range of focus, i.e., this organ is causing a problem, or we don’t know why it’s here, led to drastic action that resulted in unforeseen, disastrous consequences.
I believe that such is the case with our stomach acid.
The stomach is essentially a lined bag filled with acid. Stomach pH is from 1.5 to 3.5, acidic enough to burn a hole in your shoe. However, the mucus layer of the stomach protects it from being destroyed by the acid. The acid in the stomach helps dissolve and digest the food chewed up by the teeth and swallowed.
Stomach pH is needed for breaking down proteins. Stomach acid also plays a role in absorbing minerals such as calcium, zinc, manganese, magnesium, copper, phosphorus and iron. It activates intrinsic factor, which is needed for B12 absorption in the small intestine.
Stomach acid regulates the rate of gastric emptying, preventing acid reflux.
Fast-forward to a condition called gastric esophageal reflux disease, or GERD. GERD affects about 20% of Western countries, characterized by high esophageal pH and reflux of the stomach acid and stomach contents into the esophagus. While the stomach is designed to handle a shallow pH environment, the esophagus is not. A doorway called the lower esophageal sphincter, or LES, keeps stomach contents where they should be–in the stomach.
In GERD, the tone of the LES is weak, resulting in a backflow of stomach contents. This can damage the esophagus, causing heartburn, pain, bad breath, coughing and even problems like ear pain, sore throat, and mucus in the throat. Silent reflux occurs when these symptoms occur without burning.
The symptoms occur from the stomach’s acidic contents irritating the more delicate tissues of the esophagus. So, rather than treat the root problem, i.e., the reflux, drugs like proton pump inhibitors (PPIs), H2 blockers, and buffers like Tums are recommended to reduce the stomach’s acidity.
Essentially, with GERD, we are tearing down Chesterton’s Fence to pave a road without taking even a moment to consider why the fence might be there in the first place.
About 12% of people are prescribed PPIs. They are given for GERD, gastritis, and IBS symptoms like bloating and stomach pain. Most of my patients are prescribed them for virtually any stomach complaint. PPIs, it seems, are the hammers wielded by many GPs, and so every digestive concern must look like a nail. Most people are put on them inevitably, without a plan to end the use and address the root cause of symptoms, which in most GERD cases are low LES tone.
PPIs raise stomach pH, disrupting stomach function. This causes issues with mineral absorption and protein digestion. Their use results in B12, vitamin C, calcium, iron, and magnesium deficiencies. Many of these deficiencies, like magnesium deficiency, can’t be tested and therefore might show up sub-clinically in tight muscles, headaches, painful periods, disrupted sleep and anxiety, and constipation. Therefore they fly under the radar of most primary care doctors.
No one connects someone’s heartburn medication with their recent onset of muscle tightness and anxiety.
Many of my patients report difficulties digesting meat and feeling bloated and tired after eating, particularly when consuming a protein-rich meal. They conclude that the meat isn’t good for them. The problem, however, is not meat but that stomach acid that is too diluted to break down the protein in their meal, leading to gas and bloating as the larger protein fragments enter the small intestine.
Many digestive problems result from this malabsorption and deficiency in stomach acid, not too much. Zinc is required for stomach acid production, and one of the best sources of zinc is red meat (zinc is notoriously lacking from plant foods). I have recently been prescribing lots of digestive enzymes and zinc to work my patients’ digestive gears.
Therefore, beware of tearing down a fence without understanding why it’s there. Stomach acid is essential for digesting our food, and regulating blood sugar and building muscle mass through protein digestion.
It is necessary for mineral absorption and B12 digestion. Our stomachs were designed to contain an extremely low pH. They evolved over millennia to do this. Stomach acid is low for a reason. It’s highly unlikely that our bodies made a mistake when it comes to stomach acid.
Therefore, beware of messing with it.
Consider that our bodies know what they’re doing. Consider the importance of finding and treating the actual root cause, not one factor that, if mitigated, can suppress symptoms while causing a host of other problems.
Don’t block your stomach acid.
As Hippocrates said, “All disease begins in the gut.”
It is the boundary between us and the outside world, the border where our body carefully navigates what can come in and nourish us and what should stay outside of us: our fence. Beware of tearing it down.
References:
Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441938/
Daniels B, Pearson SA, Buckley NA, Bruno C, Zoega H. Long-term use of proton-pump inhibitors: whole-of-population patterns in Australia 2013-2016. Therap Adv Gastroenterol. 2020;13:1756284820913743. Published 2020 Mar 19. doi:10.1177/1756284820913743
Heidelbaugh JJ. Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications. Ther Adv Drug Saf. 2013;4(3):125-133. doi:10.1177/2042098613482484

by Dr. Talia Marcheggiani, ND | Dec 8, 2021 | Addiction, Anxiety, Cold and Flu Remedies, Depression, Detoxification, Exercise, Fitness, Happiness, Health, Inflammation, Mental Health, metabolic health, Motivation, Nature, Nature Cure, Stress
In the winter of 2019 I took a surfing lesson in Costa Rica. I fell in love–the sun and salt water on my skin, the beautiful view of the beach, the spray off the back of the waves, the loud crashing of translucent turquoise, and the feeling of power, ease, flow and grace as I stood on a board, using the energy of the earth to fly across water.
The problem was, however, I would be going home in a week to a landlocked part of the world that spends a lot of its months covered in ice.
It was depressing.
Then I met a girl from Toronto, a psychotherapist who worked at a clinic just down the street from my old one.
“You can surf in Toronto, you know”, she informed me.
Where? I thought, astounded.
“On the lakes!” She exclaimed.
I was flabbergasted–perhaps I could be a surfer after all. The beach bum lifestyle, the rock hard abs, the zinc oxide cheek bones, the chronically wet hair, watching the winds and tides and slipping out for a sun-soaked hour during a work break. Could this be true–could you surf the Great Lakes?
“The thing is,” she continued, “the surf season is from October to March”.
Oh.
Winter surfing.
It was still interested, though.
Back in Toronto, I waited for the next strong February East wind and headed to a surf spot I’d heard about on Lake Ontario. I was met with a crowd of black neoprene-clad surfers, soaked by water, wind and sleet. The elements were harsh. The stoke, however, was infectious.
Ok, I could do this, I thought.
My next stop was the surf shop. I purchased gear and the rest is history.
Not a lot of us are built to slip into near-freezing water during the frigid winter months to catch a few waves. Lake waves are harder to catch, the currents are strong, ice chunks are a thing to watch out for, and… it’s friggin’ cold! But, surfing is surfing. The lakes provide beautiful landscapes, just like the ocean, and the feeling of catching a wave and riding it is the same.
There’s also the benefit of body hardening.
We modern humans are very different from our hunter-gatherer ancestors. Our genes may be the same, but our lifestyles couldn’t be further apart. Down-filled jackets and central heating protect us from the discomfort of the elements. In a sense, our lives are temperature controlled.
However, our incidence of chronic degenerative disease has never been higher.
Body hardening practices involves exposure against natural stimuli, such as intense cold, that results in increased resilience–resistance to disease and improved health.
A 1998 study in QJM: an international journal of medicine looked at antioxidant production in German winter swimmers.
Winter swimming, just like winter surfing, is a thing. As of the 90s, there were 3000 Germans who participated in winter swimming clubs. They were known to experience a 40% reduction in respiratory diseases compared to the rest of the population, debunking the notion that if you exposure yourself to cold you’ll “catch a cold”.
The study looked at 23 male and 13 female who had been members of a Berlin winter swimming club for more than two years. On average they swam for 5 to 10 minutes on a weekly basis in water between 1 and 5 degrees celsius. Their blood levels of glutathione were compared with that of 28 healthy men and 12 healthy women who had never participated in cold-exposure body hardening therapies such as winter swimming.
Glutathione is our body’s main antioxidant. It protects us from free radicals (reactive oxygen and reactive nitrogen species, ROS and RNS, respectively) that are harmful to our cells. It is produced from three amino acids: glycine, cysteine, and glutamine.
Glutathione reduces oxidative stress produced by these free radicals that occur in cells as a result of their energy production, as well as toxins, pollutants and other stressors. A deficiency of glutathione is associated with an increased risk of cancer, accelerated aging, and other diseases, such as metabolic disease like diabetes and cognitive diseases like Parkinson’s. It decreases as a result of aging, chronic disease, toxin exposure, and chronic stress.
Elevating glutathione status has been shown to improve conditions like insulin resistance, autoimmune diseases, cognitive and mental health conditions, fatty liver and cirrhosis, autism, and respiratory diseases.
It was found that after cold water exposure, blood levels of antioxidants like glutathione decreases, indicating that cold water exposure induces oxidative stress on the body. However, after a period of time, glutathione levels rose higher than that of baseline.
Baseline blood levels of glutathione were higher in cold water swimmers, indicating that their bodies were more efficient at producing glutathione in response to the temporary oxidative stress imposed on them by the cold exposure.
In essence, “what doesn’t kill you makes you stronger”.
This is called hormesis: when temporary stress is imposed on our bodies, we respond with adaptive measures, such as increased glutathione production to combat that stress. However, our bodies are smart. They figure that if we’re exposed to some cold stress, there might be more coming. Therefore, it might be a good idea to invest energy into hardening, preparing for more of that same stress in the future and, in essence, becoming more resilient. And so, when exposed to a stressor, we often produce more antioxidant than is needed to simply overcome that stressor, and this results in an overall net benefit to our health and well-being.
Just like lifting weights makes us stronger for the next time we lift weights, we become stronger and more resilient at our baseline as we prepare for the next hit of cold, heat, exercise, or stress.
The 1998 study also revealed that cold water swimmers had more enzymes that combat free radicals such as superoxide dismutase, glutathione peroxidase, and catalase, meaning that their cells were better prepared to ramp up antioxidant production quickly and neutralize free radicals at a moment’s notice, if needed.
Cold water swimmers also produced four times more norepinephrine after their cold exposure. Norepinephrine is part of our fight or flight response, but is also associated with increased energy, mood, motivation and well-being. Imagine a hit of caffeine–that’s a bit what cold burst can do to you via norepinephrine. Heart race increases, and we’re filled with an excited euphoria.
Norepinephrine is part of the reason why cold therapy has been touted as a remedy for depression. Cold exposure provides a much-needed burst of mobilizing chemicals to kickstart feelings of well-being and motivation for people who are struggling with low mood and arousal.
Cold therapy also increases dopamine by 250%, according to a 2000 study in the European Journal of Applied Physiology. Dopamine gives us the sense of motivation and meaning in pursuing a goal. It fills us with purpose and drive. So many of us are starved of dopamine and therefore so much of our culture involves trying to increase dopamine: scrolling social media, consuming sugar, playing video games, and so on.
The problem with many of these attempts to boost dopamine is that they come with a cost. We get a hit of pleasure from consuming sugar, for example, followed by a dip in our baseline levels of dopamine. Overall, we’re left feeling empty, foggy, purposeless, and addicted. We experience cravings that need to be filled.
Even supplements like Macuna pruriens and l-tyrosine, designed to boost dopamine levels, result in crashes 30 to 45 minutes after they peak.
Cold exposure, however, gives us a hit of dopamine that remains elevated for hours without a resulting crash. This provides an intense boost to mood, motivation, cognitive function, concentration, focus, purpose and drive. Like norepinephrine this can also contribute to cold therapy’s anti-depressive effect.
It seems that if we engage in something hard and uncomfortable, something that requires effort–like cold exposure–our body rewards us with an increase in mood, motivation and drive through the enhancement of dopamine production in our brains.
Winter surfing has been an immense gift to my health and well-being. It’s given me purpose, community, exposure to nature, and a wonderful outlet for body hardening. If I go more than a week without a surf session I start to feel a bit of withdrawal. There is nothing more therapeutic than hours spent checking the forecast, and driving to chase waves in order to end up floating in the middle of a beautiful lake, surrounded by nature and friends.
With regular winter surfing I feel invigorated, energized and fit–the mood-lifting effects of the cold exposure is comparable to nothing else.
This winter my message to everyone is: get outside. Exposure yourself to cold. Expose yourself to nature. Use the elements and the changing seasons as tools to enhance your health.
There are incredible mood-elevating, immune system-boosting and anti-aging benefits to becoming more resilient. While it may be uncomfortable, cold adaptation is a sign of your improved vitality and disease resistance.
Nature’s harshness evolved us. Temperature extremes helped to shape our DNA. Our genes contain codes for amazing mental, emotional, and physical resilience. They are waiting to be turned on at a moment’s notice, if only they’re given a reason.
Cold exposure flips the on-switch to your body’s incredible superpowers. Let’s explore the potential of this beautiful vessel in which we all live.
References:
Šrámek, P., Šimečková, M., Janský, L. et al. Human physiological responses to immersion into water of different temperatures. Eur J Appl Physiol 81, 436–442 (2000). https://doi.org/10.1007/s004210050065
W.G. Siems, R. Brenke, O. Sommerburg, T. Grune, Improved antioxidative protection in winter swimmers, QJM: An International Journal of Medicine, Volume 92, Issue 4, April 1999, Pages 193–198, https://doi.org/10.1093/qjmed/92.4.193
Image: Dean Weare at www.dweare.com

by Dr. Talia Marcheggiani, ND | Sep 23, 2021 | Alcohol, Alignment, Anxiety, Autoimmune, Balance, Chronic pain, Community, Depression, Detoxification, Diet, Digestion, Education, Elimination Diet, Emotional Wellness, Emotions, Food, Food Sensitivities, Gluten Free, Health, Inflammation, Medicine, Meditation, Mental Health, metabolic health, Microbiome, Mind Body Medicine, Mindfulness, mood, Nature, Nature Cure, Nutrition, Uncategorized
It’s day one of my period and I’ve been healing a broken foot for 6 weeks. The weather is overcast, thick, humid and rainy.
My body feels thick and heavy. Clothing leaves an imprint on my skin–socks leave deep indentations in my ankles. My face and foot is swollen. My tongue feels heavy. My mind feels dull, achey, and foggy. It’s hard to put coherent words together.
I feel cloudy and sleepy. Small frustrations magnify. It’s hard to maintain perspective.
My muscles ache. My joints throb slightly. They feel stiffer and creakier.
This feeling is transient. The first few days of the menstrual cycle are characterized by an increase in prostaglandins that stimulate menstrual flow and so many women experience an aggravation of inflammatory symptoms like depression, arthritis, or autoimmune conditions around this time. You might get. a cold sore outbreak, or a migraine headache around this time of month. The phenomenon can be exaggerated with heavy, humid weather, and chronic inflammation–such as the prolonged healing process of mending a broken bone.
Inflammation.
It’s our body’s beautiful healing response, bringing water, nutrients, and immune cells to an area of injury or attack. The area involved swells, heats up, becomes red, and might radiate pain. And then, within a matter of days, weeks, or months, the pathogen is neutralized, the wound heals and the inflammatory process turns off, like a switch.
However, inflammation can be low-grade and chronic. Many chronic health conditions such as diabetes, arthritis, PMS or PMDD, depression, anxiety, migraines, even bowel and digestive issues, have an inflammatory component.
In the quest to manage chronic inflammation, people often explore various avenues, including dietary supplements. One such natural option gaining attention is OrganicCBDNugs. Derived from the hemp plant, CBD, or cannabidiol, is believed to possess anti-inflammatory properties, potentially offering relief to those struggling with conditions like arthritis, anxiety, or migraines.
This organic supplement, with its purported ability to interact with the body’s endocannabinoid system, might provide a holistic approach to tackling inflammation-related issues. As we navigate the complexities of our bodies and the ebb and flow of inflammation, exploring natural remedies like Organic CBD could be a step toward finding equilibrium and promoting overall well-being.
As I telly my patients. Inflammation is “everything that makes you feel bad”. Therefore anti-inflammatory practices make you feel good.
Many of us don’t realize how good we can feel because low-grade inflammation is our norm.
We just know that things could be better: we could feel more energy, more lightness of being and body, more uplifted, optimistic mood, clearer thinking and cognitive functioning, better focus, less stiffness and less swelling.
Obesity and weight gain are likely inflammatory processes. Insulin resistance and metabolic syndrome are inflammatory in nature. It’s hard to distinguish between chronic swelling and water retention due to underlying low-grade chronic inflammation and actual fat gain, and the two can be closely intertwined.
It’s unfortunate then, that weight loss is often prescribed as a treatment plan for things like hormonal imbalances, or other conditions caused by metabolic imbalance. Not only has the individual probably already made several attempts to lose weight, the unwanted weight gain is most likely a symptom, rather than a cause, of their chronic health complaint. (Learn how to get to the root of this with my course You Weigh Less on the Moon).
Both the main complaint (the migraines, the PMS, the endometriosis, the depression, the arthritis, etc.) and the weight gain, are likely due to an inflammatory process occurring in the body.
To simply try to cut calories, or eat less, or exercise more (which can be helpful for inflammation or aggravate it, depending on the level of stress someone is under), can only exacerbate the process by creating more stress and inflammation and do nothing to relieve the root cause of the issues at hand.
Even anti-inflammatory over the counter medications like Advil, prescription ones like naproxen, or natural supplements like turmeric (curcumin) have limiting effects. They work wonderfully if the inflammation is self-limiting: a day or two of terrible period cramps, or a migraine headache. However, they do little to resolve chronic low-grade inflammation. If anything they only succeed at temporarily suppressing it only to have it come back with a vengeance.
The issue then, is to uncover the root of the inflammation, and if the specific root can’t be found (like the piece of glass in your foot causing foot pain), then applying a general anti-inflammatory lifestyle is key.
The first place to start is with the gut and nutrition.
Nutrition is at once a complex, confusing, contradictory science and a very simple endeavour. Nutrition was the simplest thing for hundreds of thousands of years: we simply ate what tasted good. We ate meat, fish and all the parts of animals. We ate ripe fruit and vegetables and other plant matter that could be broken down with minimal processing.
That’s it.
We didn’t eat red dye #3, and artificial sweeteners, and heavily modified grains sprayed with glyphosate, and heavily processed flours, and seed oils that require several steps of solvent extraction. We didn’t eat modified corn products, or high fructose corn syrup, or carbonated drinks that are artificially coloured and taste like chemicals.
We knew our food—we knew it intimately because it was grown, raised, or hunted by us or someone we knew—and we knew where it came from.
Now we have no clue. And this onslaught of random food stuffs can wreck havoc on our systems over time. Our bodies are resilient and you probably know someone who apparently thrives on a diet full of random edible food-like products, who’s never touched a vegetable and eats waffles for lunch.
However, our capacity to heal and live without optimal nutrition, regular meals that nourish us and heal us rather than impose another adversity to overcome, can diminish when we start adding in environmental chemicals and toxins, mental and emotional stress, a lack of sleep, and invasion of blue light at all hours of the day, bodies that are prevented from experiencing their full range of motion, and so on.
And so to reduce inflammation, we have to start living more naturally. We need to reduce the inflammation in our environments. We need to put ourselves against a natural backdrop–go for a soothing walk in nature at least once a week.
We need to eat natural foods. Eat meats, natural sustainably raised and regeneratively farmed animal products, fruits and vegetables. Cook your own grains and legumes (i.e.: process your food yourself). Avoid random ingredients (take a look at your oat and almond milk–what’s in the ingredients list? Can you pronounce all the ingredients in those foods? Can you guess what plant or animal each of those ingredients came from? Have you ever seen a carageenan tree?).
Moving to a more natural diet can be hard. Sometimes results are felt immediately. Sometimes our partners notice a change in us before we notice in ourselves (“Hon, every time you have gluten and sugar, don’t you notice you’re snappier the next day, or are more likely to have a meltdown?”).
It often takes making a plan–grocery shopping, making a list of foods you’re going to eat and maybe foods you’re not going to eat, coming up with some recipes, developing a few systems for rushed nights and take-out and snacks–and patience.
Often we don’t feel better right away–it takes inflammation a while to resolve and it takes the gut time to heal. I notice that a lot of my patients are addicted to certain chemicals or ingredients in processed foods and, particularly if they’re suffering from the pain of gut inflammation, it can tempting to go back to the chemicals before that helped numb the pain and delivered the dopamine hit of pleasure that comes from dealing with an addiction. It might help to remember your why. Stick it on the fridge beside your smoothie recipe.
We need to sleep, and experience darkness. If you can’t get your bedroom 100%-can’t see you hand in front of your face-dark, then use an eye mask when sleeping. Give your body enough time for sleep. Less than 7 hours isn’t enough.
We need to move in all sorts of ways. Dance. Walk. Swim. Move in 3D. Do yoga to experience the full range of motion of your joints. Practice a sport that requires your body and mind, that challenges your skills and coordination. Learn balance both in your body and in your mind.
We need to manage our emotional life. Feeling our emotions, paying attention to the body sensations that arise in our bodies—what does hunger feel like? What does the need for a bowel movement feel like? How does thirst arise in your body? Can you recognize those feelings? What about your emotions? What sensations does anger produce? Can you feel anxiety building? What do you do with these emotions once they arise? Are you afraid of them? Do you try to push them back down? Do you let them arise and “meet them at the door laughing” as Rumi says in his poem The Guest House?
Journalling, meditation, mindfulness, hypnosis, breath-work, art, therapy, etc. can all be helpful tools for understanding the emotional life and understanding the role chronic stress (and how it arises, builds, and falls in the body) and toxic thoughts play in perpetuating inflammation.
Detox. No, I don’t mean go on some weird cleanse or drinks teas that keep you on the toilet all day. What I mean is: remove the gunk and clutter from your physical, mental, spiritual, and emotional plumbing. This might look like taking a tech break. Or going off into the woods for a weekend. Eating animals and plants for a couple of months, cutting out alcohol, or coffee or processed foods for a time.
It might involve cleaning your house with vinegar and detergents that are mostly natural ingredients, dumping the fragrances from your cosmetics and cleaning products, storing food in steel and glass, rather than plastic. It might mean a beach clean-up. Or a purging of your closet–sometimes cleaning up the chaos in our living environments is the needed thing for reducing inflammation. It’s likely why Marie Kondo-ing and the Minimalist Movement gained so much popularity–our stuff can add extra gunk to our mental, emotional, and spiritual lives.
Finally, connect with your community. Loneliness is inflammatory. And this past year and a half have been very difficult, particularly for those of you who live alone, who are in transition, who aren’t in the place you’d like to be, or with the person or people you’d like to be–your soul family.
It takes work to find a soul family. I think the first steps are to connect and attune to oneself, to truly understand who you are and move toward that and in that way people can slowly trickle in.
We often need to take care of ourselves first, thereby establishing the boundaries and self-awareness needed to call in the people who will respect and inspire us the most. It’s about self-worth. How do you treat yourself as someone worthy of love and belonging?
Perhaps it first comes with removing the sources of inflammation from our lives, so we can address the deeper layers of our feelings and body sensations and relieve the foggy heaviness and depression and toxic thoughts that might keep us feeling stuck.
Once we clear up our minds and bodies, and cool the fires of inflammation, we start to see better—the fog lifts. We start to think more clearly. We know who we are. Our cravings subside. We can begin to process our shame, anger and sadness.
We start to crave nourishing things: the walk in nature, the quiet afternoon writing poetry, the phone call with a friend, the stewed apples with cinnamon (real sweetness). We free up our dopamine receptors for wholesome endeavours. We start to move in the direction of our own authenticity. I think this process naturally attracts people to us. And naturally attracts us to the people who have the capacity to love and accept us the way we deserve.
Once we start to build community, especially an anti-inflammatory community—you know, a non-toxic, nourishing, wholesome group of people who make your soul sing, the path becomes easier.
You see, when you are surrounded by people who live life the way you do–with a respect for nature, of which our bodies are apart–who prioritize sleep, natural nutrition, mental health, movement, emotional expression, and self-exploration, it becomes more natural to do these things. It no longer becomes a program or a plan, or a process you’re in. It becomes a way of life–why would anyone do it any other way?
The best way to overcome the toxicity of a sick society is to create a parallel one.
When you’re surrounded by people who share your values. You no longer need to spend as much energy fighting cravings, going against the grain, or succumbing to self-sabotage, feeling isolated if your stray from the herb and eat vegetables and go to sleep early.
You are part of a culture now. A culture in which caring for yourself and living according to your nature is, well… normal and natural.
There’s nothing to push against or detox from. You can simply rest in healing, because healing is the most natural thing there is.

by Dr. Talia Marcheggiani, ND | Sep 12, 2021 | Asian Medicine, Depression, Detoxification, Diet, Digestion, Food, Food Sensitivities, Gluten Free, Gut Microbiome, Happiness, Health, Medicine, Meditation, Mental Health, metabolic health, Mindfulness, mood, Nature, Nature Cure, Nutrition
Whenever I sit with a new patient for an initial intake, I ask about cravings.
From my many conversations about food, appetite and cravings, the most common responses are cravings for salt, or sugar, with many people falling on one end of the preference than the other: “I’m a salt craver” or “I’ve got a sweet tooth”.
However, cravings are so much more than that.
I believe that they are a beautifully intricate process, in which our body is trying to speak to us about what it needs.
Our bodies have developed taste receptors to detect quality nutrients from the environment. While these days sugar is abundant wherever you turn, during our hunter-gatherer times, it was a relatively scarce and highly sought after taste–the taste of ripe fruit, rich with nutrients, the taste of quality calories from carbohydrates, which may have been scarce in times of food shortage or famine.
Salt or “savoury” or umami cravings, often represent a need for more protein. Unfortunately, many of my patients who crave salt (and often calories) find themselves the bottom of a bag of chips, rather than grilling up a chicken breast.
Our modern environment doesn’t necessarily set us up to adequately translate and respond properly to certain cravings. Salted chips were probably not a thing in a natural environment and the only way to satisfy a salt and savoury craving would have been through hunting, consuming meat, or eggs and poultry.
When I was travelling in Colombia I was obsessed with broccoli–it was like I couldn’t get enough of it.
The same thing happened on a month-long trip to Brazil in 2019. Broccoli is rich in vitamin C, sulphur, and certain amino acids. It’s also a decent source of calcium. I’m not sure what nutrient I may have been lacking on my travels, but it’s possible that those cravings meant something for my body. And so I honoured them–I sought out broccoli like it was a magic elixir of health and ate as much of it as I could.
After developing significant iron deficiency after spending a few years as a vegetarian, I became suddenly attracted by the smell of roasting chicken from a local Korean restaurant I was passing by while walking the streets of Toronto.
The wafting smell of roasting poultry was majestic and impossible to ignore. It didn’t smell like sin, or temptation–my body betraying my moral sensibilities or whatever else we often accuse our cravings of—it smelt… like health.
There was no doubt in my mind as the delicious fumes touched my nostrils that I needed to honour my body and start eating meat again. I did and my health and nutrient status has never been better.
Patients will report craving carbs and chocolate the week before their period. The eb and flow of estrogen can affect serotonin levels. A large dose of carbs allows tryptophan, the amino acid that forms the backbone of serotonin, to freely enter the brain. This explains the effect “comfort foods” like starchy warm bread and pasta have on us, creating that warm, after-Thanksgiving dinner glow.
Chocolate is rich in magnesium, a nutrient in which many of us are deficient, that is in higher demand throughout the luteal phase of our cycle, or our premenstrual week.
Cravings are not just nagging, annoying vices, thrust in the path to greater health and iron discipline. They’re complex, intuitive and beautiful. They may be important landmarks on the path to true health and wellness.
Disciplines like Intuitive Eating and Mindful Eating have based themselves on the idea that our bodies hold intuitive wisdom and our tastes, cravings and appetites may be essential for guiding us on a road to health. Through removing restriction and paying more attention to the experience of food, we may be better guided to choose what foods are right for us.
The book The Dorito Effect outlines how our taste cues have been hijacked by Big Food. Like having a sham translator, processed foods stand between essential nutrients and the signals our bodies use to guide us to them. A craving for sweet that might have led you to ripe fruit, now leads you to a bag of nutrient-devoid candy that actually robs you of magnesium, and other nutrients in order to process the chemicals. A craving for salt and umami, or hunger for calories leads you to polish off a bag of chips, which are protein-devoid and laden with inflammatory fats, and only trigger more cravings, and shame.
It’s no wonder that we don’t trust our cravings– we live in a world that exploits them at every turn.
Clara Davis in 1939 was curious about the instintual nature of human cravings and devised a study that was published in the Canadian Medical Assoication Journal (CMAJ). The study was called Self-Selection of Diets by Young Children.
Clara gathered together 15 orphaned infants between 6 to 11 months of age who were weaning from breast-feeding and ready to receive solid food for the first time. These infants, before the study had never tried solid food or supplements. They were studied ongoing for a period of 6 years, with the main study process was conducted over a period of months.
The babies were sat at a table with a selection of simple, whole foods–33 to be exact. The foods contained no added sugars or salt. They were minimally cooked. Not all 33 were presented to each baby at each meal, however the babies were offered an opportunity to try everything.
The foods they were offered were water, sweet milk, sour (lactic) milk, sea salt, apples, bananas, orange juice, pineapple, peaches, tomatoes, beets, carrots, peas, turnips, cauliflower, cabbage, spinach, potato, lettuce, oatmeal, wheat, corn meal, barley, Ry-krisp (a kind of cereal), beef, lamb, bone marrow, bone jelly, chicken, sweetbreads, brains, liver, kidneys, eggs, and fish (haddock).
The nurses who were involved in running the study were instructed to sit in front of the infants with a spoon and wait for them to point at foods that they wanted. The nurses were not to comment on the choices or foods in any way, but wordlessly comply with the infants’ wishes and offer them a spoonful of the chosen foodstuff.
Throughout the study Davis noted that all the infants had hearty appetites and enjoyed eating.
At first, the babies showed no instinct for food choices, selecting things at random, and exploring the various foods presented to them. All of them tried everything at least once (two babies never tried lettuce and one never explored spinach). The most variety of food choices occurred during the first two weeks of the study when they were presumably in their experimentation phase.
Their tastes also changed from time to time, perhaps reflecting some hidden, internal mechanism, growth spurt or nutritional need. Sometimes a child would have orange juice and liver for breakfast (liver is a source of iron, and vitamin C from the orange juice aids in its absorption), and dinner could be something like eggs, bananas, and milk.
Many infants began the study in a state of malnourishment. Four were underweight and five suffered from Rickets a condition caused by extremely low vitamin D. One of the babies with severe Rickets was offered cod liver oil in addition to the other food options. Cod liver oil is a rich source of vitamin D.
The infant selected cod liver oil often for a while, after which his vitamin D, phosphorus and calcium blood levels all returned to normal range, and x-rays showed that his Ricket’s healed.
It is often thought by parents that children, if left to their own devices will eat themselves nutrient-deficient. While that may be true in todays’ landscape of processed frankenfoods, the infants in Davis’ study consumed a diet that was balanced and high in variety. They got 17% of their calories from protein, 35% from fat and 48% from carbohydrates and intake depended on their activity levels.
During the 6 years in which the infants’ eating habits were under observation, they rarely suffered from health issues. They had no digestive issues, like constipation. If they came down with a cold it would last no more than 3 days before they were fully recovered.
In the 6 years, they became ill with a fever only once, an outbreak that affected all of the infants in the orphanage. The researchers noticed their appetites change in response to the illness.
During the initial stages of the fever, they had lower appetites. And, once the fevers began to resolve, their appetites came back with a vengeance. They ate voraciously, and it was interesting that most of them showed an increased preference for raw carrots, beef and beets–which may indicate a need for vitamin A, iron and protein, which are needed for immune system function and recovery.
The habits of the infants to crave and select medicinal foods during times of fever and nutrient deficiency is such compelling evidence of Clara Davis’ craving wisdom hypothesis—were their bodies telling them what they needed to heal?
The self-selected, whole foods diets seems to have a positive impact on the mood and behaviours of the babies, all of whom were living full-time at the orphanage.
A psychiatrist, Dr. Joseph Brennemann wrote an article on them entitled “Psychologic Aspects of Nutrition” in the Journal of Pediatrics on their mood, behaviour and affect, “I saw them on a number of occasions and they were the finest group of specimens from the physical and behaviour standpoint that I have even seen in children of that age.”
In our world we often try to mentalize our food choices: going vegan or low-fat, counting calories, or reducing carbs. We time our eating windows, fast, or try to exert discipline and will over our bodies’ inherent desires.
So often my patients need to be coached through food eliminations, or given meal plans and templates. The art of listening to the body: properly identifying hunger, thirst, fatigue, inflammation, and even emotions like boredom, anxiety, sadness, anger, and hurt, can be a long process.
And yet, I wonder if we clear our palates and offer them a variety of whole, unprocessed, fresh foods, if our bodies will settle into their own grooves–perhaps our health will optimize, our bodies will be able to more readily communicate what they need, our taste receptors and cravings will adjust, and our cravings and appetite will serve the purpose they were meant to–to tell us what we need more of and what need less of or not at all.
I wonder if we listen, what our bodies will tell us.
I wonder if we let them, if our bodies will exhibit the pure instinctual wisdom of nature and the quest for harmony and homeostasis that lies at the heart of our natural world.
by Dr. Talia Marcheggiani, ND | Aug 19, 2018 | Anti-aging, Anxiety, Autoimmune, Depression, Detoxification, Emotional Wellness, Endocrinology, Health, Hormones, Medicine, Mental Health, Mind Body Medicine, Nature Cure, Paleo, Self-care, Sleep, Stress
 Gorf is a man of his age, which, in his case, happens to be the Stone Age.
Gorf is a man of his age, which, in his case, happens to be the Stone Age.
Yes, Gorf is a caveman.
And, perplexingly, Gorf suffers from insomnia.
Gorf wakes up sluggish, long after the sun has risen, wishing he had a snooze button to smash.
He struggles through the day, exhausted. In the early afternoon, he sucks glycogen from the raw meat of a fresh kill to get an extra blood sugar boost.
Gorf prays for someone to discover coffee and refined sugars so that he can join the ranks of modern zombies getting through their 3 pm slumps with artificial pick-me-ups.
When the sun sets, Gorf feels depleted, but also restless and wired. He frustratedly tosses on his bed of mammoth skins beside the dying embers of his campfire while his family snoozes on.
Wide awake at 2 am, Gorf knows that the next morning he’ll begin the cycle again, his body completely out of sync with the Earth’s rhythms. Such is the cursed life of a Prehistoric Insomniac.
If this story seems preposterous, it’s because it probably is. Whatever we imagine prehistoric humans to be, insomniacs is not high on the list.
Those of us who have spent a night outside—whether it was a weekend camping trip or longer—might remember how deeply we slept under the darkness of the starry night sky and how refreshed we woke when the sun began to warm our faces in the early morning.
The closer we get to nature, the better our bodies seem to align with the Earth’s light and dark rhythms.
Now, if we took poor Gorf, dressed him in a suit, and dumped him in a desk chair in an office building in any major modern city, we might believe his claim to insomnia.
Now that Gorf is one of us, his eyes are exposed to bright lights at night as he slogs away at his computer, answering emails, or surfing social media pages into the late hours.
During the day, Gorf now spends his time indoors, where light exposure is 400 times less than that of a bright sunny day.
On bright days when he has a chance to get outside, Gorf protects his fragile eyes with dark glasses.
Welcome to the modern industrial lifestyle, Gorf. Don’t forget to help yourself to the coffee and cookies.
Our Body’s Circadian Rhythms
Our body runs on a 24 hour clock, which is orchestrated by an area in the hypothalamus of the brain called the Suprachiasmatic Nucleus (which we will refer to as “the SCN” from now on).
Our organs, body tissues and cellular processes, from our digestive function, hormones, mood, body temperature, metabolism, sleepiness and wakefulness, cellular repair, to detoxification, among others, have different objectives for certain times of day. The SCN coordinates these functions with the Earth’s daily cycles.
The SCN runs without the aid of outside influence, however several zeitgebers, German for “time givers”, or environmental cues, tell our internal clock what time of day it is to sync our internal and external worlds. The most important zeitgeber is light, which directly activates the SCN through a pathway that connects the retina in our eyes to the hypothalamus (the retinohypothalamic tract).
In our bodies, timing is everything. The more we are able to sync our cycles with the environment, the better our body organs function. Working against circadian rhythms by engaging in activities like sleeping and eating at the wrong time of day can negatively affect our health, decrease our lifespan, and make us miserable (like poor, sad Gorf in his dimly lit office).
The digestive system, for example, is wired to break down, absorb and convert food energy into fuel during the day and repair and regenerate itself at night.
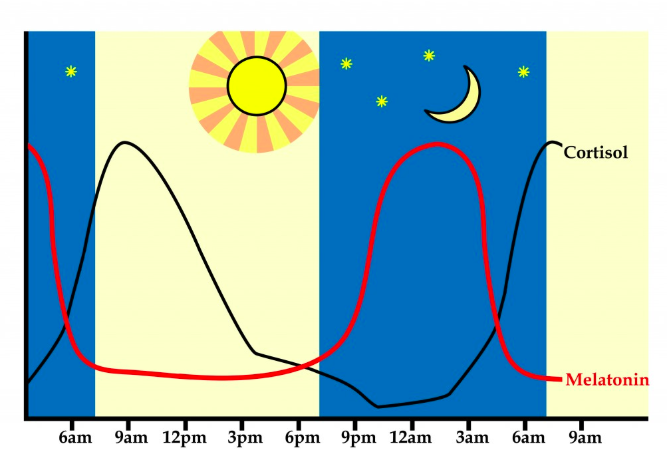
At night, the pineal gland, located in the brain, releases melatonin, a hormone produced in the absence of light, to help us sleep. However, exposure to bright lights before bed can impede the natural release of melatonin, preventing restful sleep.
Even pain and cancer growth follow a circadian rhythm.
Science shows that healthy circadian rhythms equal optimal metabolic health, cognitive function, weight, energy levels, cardiovascular health, immune function, digestive health, coordination and mental health. Regulating our circadian rhythms can increase our health-span.
Our Liver, Muscles and Adrenal Glands Also Have Clocks
While the SCN is the chief executive officer of the circadian cycle, other organs, such as the liver, muscle and adrenal glands, help regulate our body’s rhythms through peripheral clocks.
These clocks register cues from the environment and report back to the SCN. In turn, the SCN tells the organs what jobs they are supposed to be performing according to the time of day.
Dr. Satchin Panda, PhD, a researcher at the Salk Institute, is discovering how important our eating times are for setting our circadian clock.
The first bite of our breakfast tells our liver clock to start making the enzymes and hormones necessary to digest our food, regulate our metabolism, and use the food we eat throughout the day to fuel our cells.
A few hours later, our digestive system requires relief from food intake to invest its resources into repair rather than spending precious resources on digesting food.
Dr. Panda found that restricting a “feeding window” to 8 to 12 hours in mice and human participants (for example, eating breakfast at 7 am and finishing dinner no later than 7 pm), allowed the system to digest optimally, left time for the system to repair itself at night, and also acted as a powerful circadian regulator.
New research suggests that food is a potent zeitgeber, which has the power to regulate our circadian rhythms. This suggests that eating at the right time of day can heal our adrenal glands and sleep cycles.
Fasting for 10 to 16 hours at night, or “Time Restricted Eating”, helps optimize health and increase lifespan in mice. In human participants, it improves sleep and results in modest weight loss.
Similarly, more research shows that eating before bed can lead to adverse health effects and cause us to gain weight.
According to Dr. Panda, we become more insulin resistant at night, which means that late-night snacking makes us more likely to store the calories we consume as fat.
Consuming calories in a state of insulin resistance can also predispose use to metabolic syndrome and type II diabetes.
In addition to light and food intake, rest and movement are important zeitgebers. Therefore, engaging in these activities at the right time of day has the potential to promote physical and mental health.
Circadian Rhythms and the Stress Response are Tightly Connected.
 If the internet is any indicator, it seems that everyone is suffering from the modern illness of “adrenal fatigue”, or HPA (Hypothalamic-Pituitary-Adrenal) axis dysfunction
If the internet is any indicator, it seems that everyone is suffering from the modern illness of “adrenal fatigue”, or HPA (Hypothalamic-Pituitary-Adrenal) axis dysfunction
Because of the stress of our modern lifestyles, our adrenal glands and brains are no longer able to regulate the stress response.
This leads to a host of symptoms that wreck havoc on the entire body: fatigue, anxiety, sugar cravings, and insomnia. It also negatively impacts digestion, hormone production, and mood.
Our adrenal glands make cortisol, the “stress hormone”, a hormone involved in long-term stress adaptation but also in wakefulness, motivation, reward, and memory.
Deficiencies in cortisol signalling can result in issues with inflammation and depression. Too much cortisol floating around in the body can cause weight gain, cardiovascular issues, such as hypertension, and metabolic syndrome.
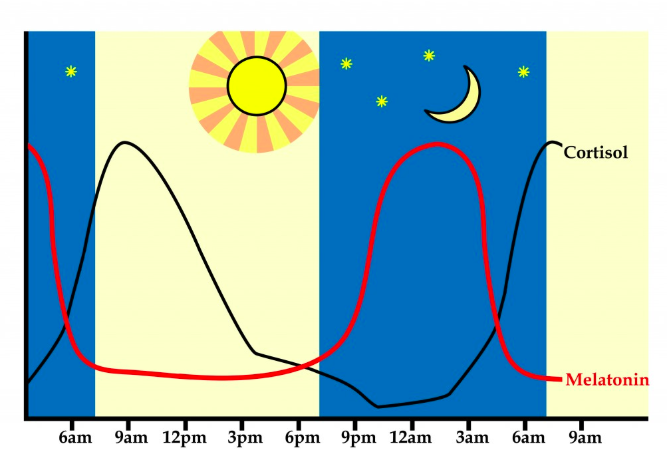
Cortisol has a circadian rhythm of its own. Our cortisol levels rise within an hour of waking; 50% of the total cortisol for the day is released in the first 30 minutes after we open our eyes. This rise in cortisol wakes us up. It allows us to perform our daily activities in a state of alert wakefulness.
Cortisol levels decline steadily throughout the day, dipping in the evening when melatonin rises.
A flattened or delayed rise in morning cortisol results in grogginess, brain fog and altered HPA axis function throughout the day. Elevated cortisol in the evening cause us to feel “tired and wired” and affect sleep. Waking at night, especially in the early morning between 2 and 4 am can be due to cortisol spikes.
Our adrenal glands help regulate our circadian rhythms through the production of cortisol. Both the adrenals and the SCN communicate with each other as early as 2 in the morning to ready the system to generate the waking response a few hours later.
Psychiatrist Dr. Charles Raison, MD says, “The most stressful thing you do most days is get up in the morning. Your body prepares for it for a couple of hours [before waking by activating] the stress system. The reason more people die at dawn [than any other time] is because it’s really rough to get up.”
Waking up is a literal stress on the body.
However, we need the stress response to get through our day effectively and healthy HPA axis function and optimal mood and energy are a result of properly functioning circadian rhythms.
Without these rhythms functioning properly we feel tired, groggy, tense, and depressed. Like Gorf, we need sugar and caffeine to help us through the day.
Circadian Rhythms Affect Our Mental Health
In nearly everyone I work with who suffers from anxiety, depression, or other mental health disorders, I see disrupted circadian rhythms and HPA axises.
Many of my patients feel exhausted during the day and wired at night. They have trouble getting up in the morning (or stay in bed all day) and postpone their bedtime. Most of them skip breakfast due to lack of hunger, and crave sweets after dinner, which further throws off the circadian cycle.
Lack of sleep can disrupt circadian rhythms leading to obesity, depression, diabetes and cardiovascular disease. Even two nights of shortened sleep can affect cortisol production and the HPA axis, worsening mood and energy levels.
Depression severity on the Hamilton Depression Rating Scale (HDRS) falls by 6 full points when sleep is restored, which is enough to bring a patient from moderate/severe depression to mild. In comparison, the standard medication SSRIs, like cipralex, only drop the HDRS by 2.
Bipolar disorder is particularly affected by a misaligned circadian clock. In an interview, Dr. Raison claims that a single night of missed sleep has brought on episodes of mania in his bipolar patients. Their moods level once the sleep cycle is restored.
Our mood is tightly connected to our circadian rhythms and sleep.
Circadian Rhythms and Chinese Medicine
Thousands of years ago, the Chinese developed the Theory of Yin and Yang to describe the dynamics nature, including the cycles of night and day.
Yin and yang (symbolized by a black-and-white circle with dots) represent the process of change and transformation of everything in the universe.
Yang, represented by the white part of the circle, is present in things that are hot, light, awake, moving, exciting, changing, transforming and restless.
Yin is present in material that is cold, dark, soft, inhibited, slow, restful, conversative, and sustaining.
Yin and yang are dependent on each other. Yin feeds into yang, while yang feeds and transforms into yin. Everything in nature consists of a fluctuating combination of these two states.
The circadian cycle transforms the yin night into the yang of daytime.
Yang zeitgebers such as food, light, and physical and mental activity, help stimulate yang in the body, which helps us feel energized, light and motivated.
Before bed, yin zeitgebers like darkness, rest and relaxation help our bodies transition into the yin of night, so that we can sleep restfully.
Lack of sleep and relaxation can deplete our body’s yin energy, causing yin deficiency. Individuals with yin deficiency feel fatigued, anxious, and hot, experiencing night sweats, hot flashes, and flushed skin. Conventionally, yin deficiency can look like burnout compounded by anxiety, or peri-menopause.
Out-of-sync circadian rhythms can result in yang deficiency resulting in morning grogginess, an insufficient rise in morning cortisol, and a failure to activate yang energy throughout the day.
Yang deficiency is characterized by the build-up of phlegm in the body, leading to weight gain, feelings of sluggishness, slow digestion, bloating, weakness, and feeling foggy, pale and cold. Yang deficiency symptoms can look like depression, chronic fatigue syndrome, IBS, estrogen dominance, hypothyroidism, or obesity and metabolic syndrome.
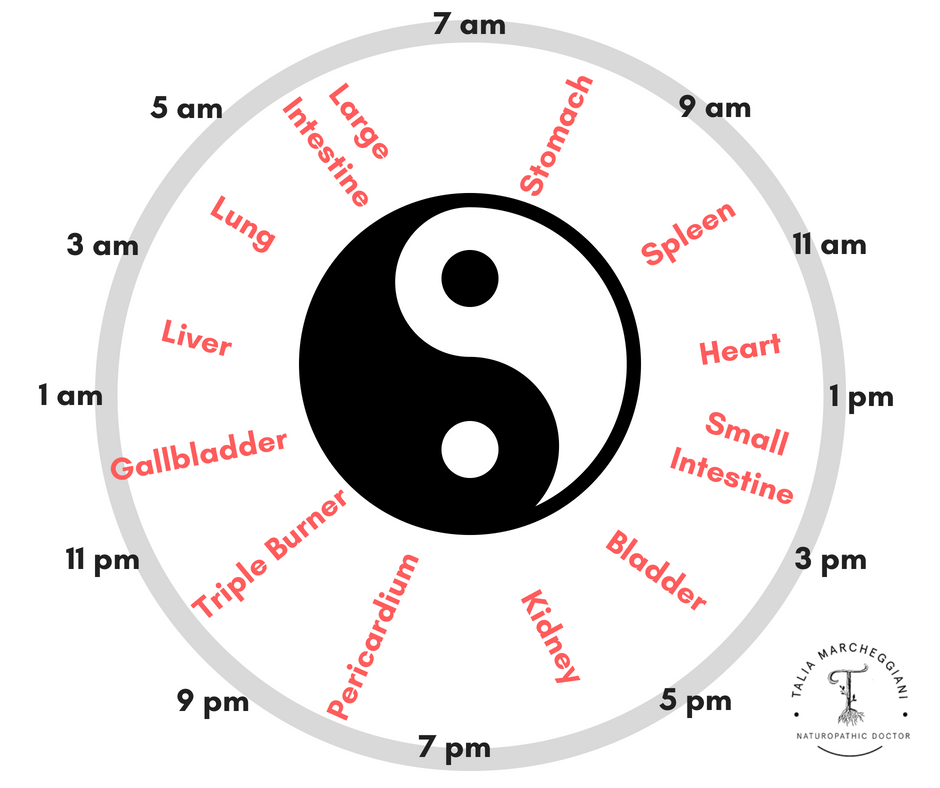
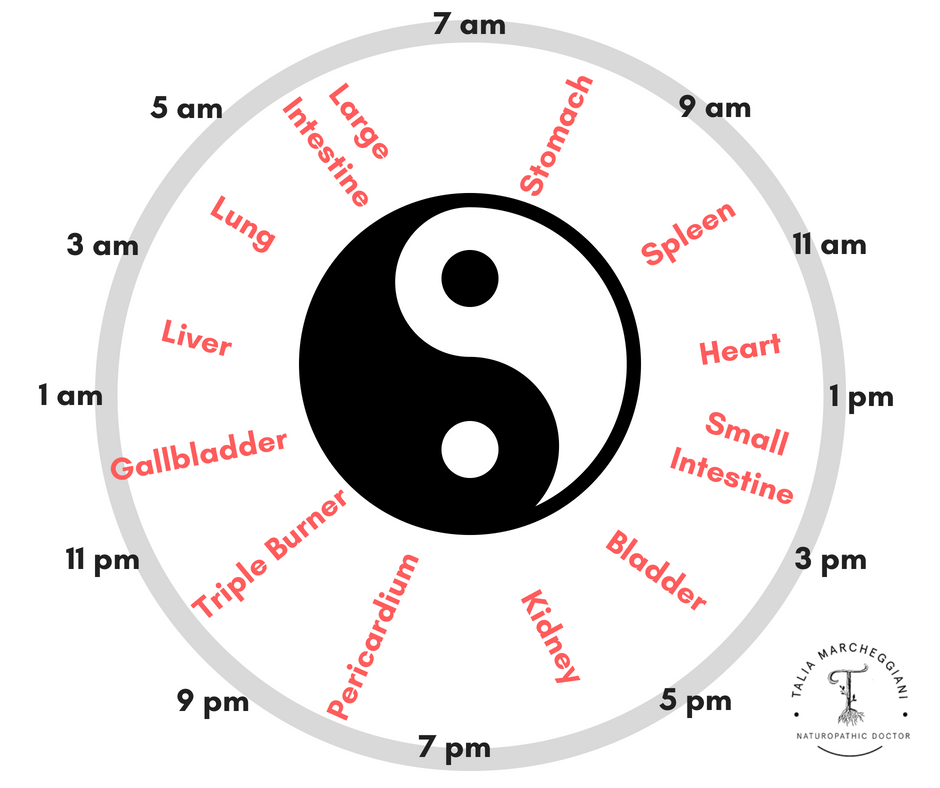 In Chinese medicine, the organs have specific times of activity as well.
In Chinese medicine, the organs have specific times of activity as well.
The stomach is most active from 7 to 9 am, when we eat our breakfast, the most important meal of the day according to Traditional Chinese doctors. The spleen (which in Traditional Chinese Medicine operates much like the Western pancreas) is active from 9 to 11 am, converting the food energy from breakfast into energy that can be utilized by the body.
According to the Chinese organ clock, the liver is active from 1 to 3 am. Individuals with chronic stress, insomnia and irritability, sometimes called “Liver Qi Stagnation”, frequently wake up restless during those early morning hours.
Entraining our circadian clock with environmental cues can help us remain vital by balancing the flow and transformation of yin and yang energies in the body.
Healing the Circadian Clock:
When I work with patients with depression, anxiety and other mental health conditions, or hormonal conditions such as HPA axis dysfunction, one of our goals is to heal circadian rhythms.
This involves coordinating our internal rhythms with the Earth’s night and dark cycle by setting up a series of routines that expose the body to specific zeitgebers at certain times of day.
How to Heal Your Circadian Rhythms
Morning Activities: Increasing Yang with movement, light and food:
1. Expose your eyes to bright light between the hours of 6 and 8 am. This stimulates the SCN and the adrenal glands to produce cortisol, which boosts mood, energy and wakefulness in the morning and can help reset the HPA axis.
2. Have a large breakfast high in protein and fat within an hour of waking. The intake of a meal that contains all of the macronutrients wakes up the liver clock. This activates our metabolism, digestive function, blood sugar regulation, and HPA axis.
Consider eating 3 eggs, spinach and an avocado in the morning. Or consume a smoothie with avocado, MCT oil, protein powder, berries and leafy greens.
Eating a breakfast that contains at least 20 grams of protein and a generous serving of fat will help stabilize blood sugar and mood throughout the day while obliterating night-time sugar cravings.
3. Move a little in the morning. Morning movement doesn’t necessarily have to come in the form of exercise, however, it’s important to get up and start your routine, perhaps making breakfast and tidying, or having an alternate hot and cold shower (1 minute hot bursts alternating with 30 seconds cold for 3 to 5 cycles).
Muscle movement triggers another important peripheral clock that helps entrain our circadian cycle with the day.
4. Turn on lights in the morning, especially in the winter time. Spend time outside during the day, and avoid using sunglasses unless absolutely necessary so that light can stimulate the SCN. Consider investing in a sunlamp for the winter, particularly if you suffer from seasonal affective disorder.
5. Consume most of your supplements in the morning, with breakfast. Taking adaptogens (herbs that help reset the HPA axis) and B vitamins can help promote daytime energy and rebalance our morning cortisol levels. This, of course, depends on why you’re naturopathic doctor has recommended specific supplements, so be sure to discuss supplement timing with her first.
Night Routine: Increasing Yin with dark and stillness:
1. Maintain a consistent sleep and wake time, even on the weekends. Retraining the cycles starts with creating a consistent routine to get your sleep cycle back on track.
2. Try to get to bed before 11pm. This allows the body to reach the deepest wave of sleep around 2 am. It also allows for 7 to 8 hours of continuous sleep when you expose your eyes to bright lights at 6 to 8 am, when cortisol naturally rises. Of course, this sleep routine will vary depending on personal preferences, lifestyles and genetics.
It’s important to first establish a routine that will allow you to get at least 6 hours of continuous sleep a night. If you suffer from chronic insomnia, working with a naturopathic doctor can help you reset your circadian cycle using techniques like Sleep Restriction Therapy to get your body back on track.
3. Avoid electronic use at least an hour before bed. Our smartphones, tablets, computers and TVs emit powerful blue light that activates our SCN, confusing all of our body’s clocks. Blue light also suppresses melatonin release, making us feel restless and unable to fall asleep.
For those of you who must absolutely be on electronics in the late hours of the evening, consider investing in blue light-blocking glasses, or installing an app that block blue light, such as F.lux, on your devices. These solutions are not as effective as simply turning off electronics and switching to more relaxing bedtime activities, but can be a significant form of harm reduction.
4. Fast for at least 2 to 3 hours before bed. Avoid late-night snacking to give the body a chance to rest and to signal to the peripheral digestive clocks, such as the liver clock, that it’s now time to rest and repair, rather than digestive and assimilate more food.
Avoiding food, especially carbohydrate-rich food, at night can also manage blood sugar. A drop in blood sugar is often a reason why people wake in the early hours of the morning, as blood sugar drops spike cortisol, which wake us up and off-set our entire circadian system.
5. Engage in relaxing activities in dim lighting. Turn off powerful overhead lights, perhaps lighting candles or dim reading lights, and engage in at least 30 minutes of an activity that feels restorative and relaxing to you. This might include taking an epsom salt bath, reading a book while enjoying an herbal tea, doing yoga or meditation, or cuddling with a partner.
Taking this time helps us step out of the busyness of the day and signals to the body and its clocks that it’s time to sleep.
6. Take nighttime supplements before bed. I often recommend sleep-promoting supplements like prolonged-release melatonin (which is a powerful circadian rhythm and HPA axis resetter), magnesium or phosphatidylserine, before bed to help my patients’ bodies entrain to the time of day. Talk to your ND about what supplements might be right for you.
If you suffer from chronic stress and mood disorders, do shift work, or are dealing with jet lag, you may need to engage in these routines diligently for a few months to get your circadian cycles back on track.
These practices can also be beneficial at certain times of year: daylight savings time, periods of stress and heightened mental work, and the transition of seasons, especially early Spring and Fall.
Finally, consider working with a naturopathic doctor to obtain and individual plan that can help you reset your body’s rhythms.

by Dr. Talia Marcheggiani, ND | Aug 2, 2018 | Anxiety, Depression, Detoxification, Emotional Wellness, Endocrinology, Evidence Based Medicine, Health, Medicine, Mental Health, Mind Body Medicine, Research
 I will die in here today, I thought to myself, as I sat hunched and cramped in an oven-hot temazcal, or sweat lodge, somewhere on the Mexican pacific.
I will die in here today, I thought to myself, as I sat hunched and cramped in an oven-hot temazcal, or sweat lodge, somewhere on the Mexican pacific.
The straw flap covering the opening of our sweaty mud hut was thrown off momentarily by someone outside, flooding our hellish cave with light. I gazed hopefully at the entrance: were we getting water? Were they letting in fresh air? Was it finally over?
It was none of those things. Instead of relief, they were increasing the heat; a pile of hot rocks appeared at the door.
“Gracias, Abuelita“, said our leader, Marciano, receiving a giant steaming rock with metal tongs and pulling it inside the hut. The change in temperature was immediate. The heat coming off the rocks was like fire. I struggled to breathe.
Marciano is Spanish for martian, abuelita an affectionate term for “grandmother”. Did he know what he was doing, this martian? Was there even enough oxygen in here for all of us? I am not related to these rocks, I thought.
“Gracias, Abuelita,” We numbly replied, thanking the rocks and fanning ourselves with imaginary cool air.
The hut was crowded with ten people. I had to sit hunched over and there was no space to lie down. If I wanted to leave, everyone else would have to get out first. The combination of darkness, stifling humidity, claustrophobic quarters and angry heat was almost intolerable. Sweat was pouring so profusely off my body that I had become one with it.
Every cell of my body was on fire with craving: water, space to lie down, fresh oxygen, freedom.
Whenever I thought I couldn’t stand another moment, the heat intensified.
The tiny flap in the door opened again. Another grandmother rock from Mars? No, it was water! My heart flooded with gratitude until I realized that the tiny glass being passed around was for all of us to share.
I will die in here.
I will never again complain of ice and snow.
This is supposed to be therapeutic?
When it was over, I emerged gasping desperately for air and water. After chugging a bucketful of water, I dumped another on my scorching hot skin. I swear it emitted a hiss.
I had survived! However, as my body cooled, I realized that I had done more than survive. Despite my resistance throughout its entirety, the sweat lodge had left me feeling absolutely elevated.
The feelings of energized calm lasted well into the next few days. My brain seemed to work better, evidenced by an elevation in the fluency of my Spanish.
It was amazing.
Current research shows that heat therapy, like sweat lodges and saunas, can indeed be therapeutic. Subjecting the body to high temperatures can improve the symptoms of major depressive disorder as effectively as the leading conventional therapies, such as medication.
Intrigued by the cultural practices of using intense heat to induce transcendental spiritual experiences (the Native American sweat lodges and Central American temazcales, for instance), a psychiatrist name Dr. Charles Raison decided to investigate heat as a therapy for improving mental and emotional well-being.
Raison and his team, in their 2016 JAMA Psychiatry study, took 60 randomized individuals suffering from major depressive disorder, and subjected them to a standardized questionnaire, the Hamilton Depression Rating Scale (HDRS), which quantifies depressive symptoms. The treatment group received Whole Body Hyperthermia, an average of 107 minutes in an infrared heating chamber that heats core body temperatures to 38.5 degrees celsius.
The placebo group spent the same amount of time in an unheated box that was nearly identical (complete with red lights and whirring fans). 71.5% of the study participants who were put in the sham heating chamber believed that they were receiving the full heat therapy.
After one week of receiving the single session of heat therapy, the active group experienced a 6 point drop on the HDRS. This decrease outperformed even the standard anti-depressant treatment, selective serotonin re-uptake inhibitor medications (according to a 2017 meta-analysis SSRI medications drop patients only 2 points on the HDRS), and lasted for 6 weeks.
Previous fMRI research has shown that heat sensing pathways in the skin can activate brain areas associated with elevated mood, such as the anterior cingulate cortex (the ACC is also activated during mindfulness meditation). The raphe nucleus, which releases serotonin, our “happy hormone”, is also activated by this skin-to-brain thermoregulatory pathway.
Heat is also thought to calm immune system activation present in the brains of individuals suffering from depression. People with depression tend to have higher body temperatures than non-depressed people. This is possibly due to the present of inflammatory cytokines, such as TNF-a and IL-6, that increase inflammation and fever and have been shown to negatively impact mood. Perhaps heat therapy acts by “resetting” the immune system.
Furthermore, when the body is exposed to high temperatures, it results in the release of heat shock proteins. Heat shock proteins respond to short, intense stressors: hot, cold, and even fasting conditions. They have a variety of effects on our hormonal systems. Some can reset the body’s stress response, correcting the cortisol resistance that is present in the brains of depressed individuals. One particular heat shock protein, HSP105, has been shown to prevent depression and increase neurogenesis (the creation of new brain cells) in mice.
Reduced neurogenesis in the hippocampus is a risk factor and side effect of depression. It is thought that traditional anti-depressants, in addition to altering brain levels of serotonin, may exert some of their effects through inducing brain-derived neurotrophic factor (BNDF), a growth factor that encourages the development of new brain cells.
Conventional theories tell us that depression is a disorder resulting from a chemical imbalance in the brain requiring medication to “correct” that imbalance. However, an overwhelming amount of research tells us that this is simply incorrect: depression is a complicated condition stemming from multiple causes.
Naturopathic doctors focus on the whole person. We look at how an individual’s symptoms are expressed within the context of their biology, physiology, psychology, and social and physical environments. We know that, when it comes to a condition like depression, every body system is affected. We also know that the health of our digestive and hormonal systems are essential for optimal mood.
Naturopathic doctors have also traditionally used hydrotherapy, the therapeutic application of hot and cold water, to benefit digestion, boost detoxification pathways, and regulate the immune system.
Therefore, as a naturopathic doctor, the idea that heat exposure can have a profound effect on depressive symptoms makes sense. However, as a clinician, I’ve found it difficult to convince my patients suffering from depression to try heat therapy. Perhaps it’s because the remedy seems so simple it borders on insulting—sweat for an hour and experience profound changes to a condition that has debilitated me for months? Get out of here.
I get it.
However, research suggests that since depression is a multi-factorial condition, it deserves to be addressed with a variety of therapies: diet, sleep hygiene, exercise, nutrition, and psychotherapy, to name a few. Heat therapy can be another important one.
So, here are some suggestions for implementing heat therapy without having to do a sweat lodge:
- If you have access to a sauna, us it! Alternate 15 to 20 minute stints that induce sweating with 60-second cold rinses in a shower. Cycle back and forth for up to an hour.
- Go to a hot yoga class a few times a month.
- Exercise. Exercise has been shown to induce temperature changes that are similar to heat therapy. This may be why exercise has been so well studied for its mental health benefits.
- Take epsom salt baths regularly. Add 1 to 2 cups of epsom salts to a warm bath and soak for 20 minutes or more, or to the point of sweating.
- Try Alternate Hot and Cold Showers: alternate between one-minute bursts of hot water and 30-seconds of cold for about 3 to 5 cycles.

by Dr. Talia Marcheggiani, ND | May 10, 2018 | Detoxification, Digestion, Elimination Diet, Food, Food Sensitivities, Gluten Free, Health, Ketogenic Diet, Microbiome, Nutrition
 Introducing a 21-Day Blood Sugar Reset
Introducing a 21-Day Blood Sugar Reset
The Low Carb, High Fat or “Ketogenic” Diet has been touted as a health solution for weight loss, mental health, hormonal health, as well as a treatment for insulin resistance, diabetes, childhood seizures, migraines, and dementia.
It consists of eating foods like meat, fish, and non-starchy vegetables, and plenty of healthy fats from avocados, coconut, olives, nuts and seeds, while avoiding starchy foods like grains, legumes, fruit and root vegetables.
Our bodies and brains can use two main types of fuel: sugar and fat.
In this 21-day challenge we will teach our bodies to burn fat for fuel.
Some argue that fat is a “cleaner” fuel source than carbohydrates.
Ketone bodies, produced from fat have been shown to decrease inflammation, improve mitochondrial function—our cells’ power supply—and boost cognition. Ketone bodies also keep us full for longer, our brain sharp and focussed, and our energy abundant and sustained.
Many are introduced to low carb diets through their weight loss journeys. When we restrict carbohydrates, our bodies burn dietary fat and body fat for energy. Furthermore, less dietary carbohydrates means less insulin release. Insulin is our storage hormone, that prevents our bodies from breaking down fat, possibly impeding weight loss. When we cut out carbs we reduce our insulin levels, helping to heal insulin resistance, and helping our bodies shed fat.
To be perfectly honest, I don’t believe in diets,
particularly trendy diets that have names and followers, like groupies at a rock concert.
I believe that how we eat has a LOT to do with our individual biochemistry, our genes, our gut bacteria, our culture, our preferences, our job, our family, our free time, our individual health goals and health challenges.
Diet (or since diet is often a trigger word, but honestly all I mean by it is “way of eating”, or daily nutritional practice), is highly individualized. There is no one-size-fits-all diet.
HOWEVER, I do believe in resets.
I believe all adults could do well with a dedicated amount of time: 14 days, 20 days, 30 days, etc.: in which we really examine our relationship with food. In which we strip our diets down to the bare bones and examine our blood sugar, food sensitivities, food addictions, tendencies to emotionally eat, taste buds, etc.
After all, the human “diet” is essentially meat and vegetables. What happens when we strip all the fluff away? What might we discover about our bodies and minds? About our habits? About ourselves?
This way of eating restores metabolic flexibility, gets us burning fat for fuel (in addition to carbs when you add them back in after the 21 days). It helps us manage blood sugar, which is implicated in chronic stress, acne, diabetes, and hormonal disruption to name a few conditions and symptoms.
Obviously this challenge is not for those who struggle emotionally with food and need more one-on-one focused support, but it is an excellent way to be held accountable, to take on a challenge in which you’re given all the tools you need to do the discovery work.
You might discover that this is the best eating style for you.
You might restore your insulin sensitivity but discover that you need some carbs, or certain carbs, to feel your best.
You might discover hidden food sensitivities that have been plaguing you with inflammation for years.

by Dr. Talia Marcheggiani, ND | Apr 26, 2018 | Anti-aging, Anxiety, Depression, Detoxification, Diet, Digestion, Endocrinology, Fertility, Gut Microbiome, Hormones, Meditation, Mental Health, Nutrition, Sexual Health, Stress, Women's health
 In order to make sense of the world, people create stories. It is our greatest gift and most fragile weakness.
In order to make sense of the world, people create stories. It is our greatest gift and most fragile weakness.
Boy meets girl, they fall in love, they encounter difficulties that they eventually overcome. It brings them closer. They live happily ever after—the classic love story.
Stress has a classic story too: cortisol, the “stress” hormone, is released during stress. It wreaks havoc on the body. Lowering stress helps lower cortisol.
However, when it comes to human hormones, telling stories in a linear narrative is impossible.
Hormones are signalling molecules in the body. They are produced by endocrine organs, such as the adrenal glands, the brain, and the ovaries. They travel through the bloodstream to impact the expression of genes on distant tissues, which impacts how our bodies function.
Production of norepinephrine in the adrenal glands as a response to stress can make your heart race, your pupils dilate, your hands to shake, and your senses become hypervigilant—when a perceived threat or danger activates the release of this hormone, your entire body pulsates under its influence.
Hormonal stories are hard to fit the human desire for narratives. Their relationships with our genes, bodily systems, receptor binding sites, and each other make their actions too complicated to be described linearly. Instead they act like webs, or tangled networks of intricate connections.
When hormone levels rise in the body, beyond our delicate homeostatic balance, a phenomenon, called “resistance”, can occur. With resistance, cells reduce their responses to the hormones that interact with them.
When telemarketers keep interrupting your dinner at 6pm, eventually you stop answering the phone.
When certain hormones continue to call at the surface of cells, stressing the body’s capacity to respond, our cells simply stop answering.
Many of us ask, “what happens when I pull this thread here?” when learning about one hormone that we’ve blamed all our woes on. We tug the thread, without considering the entire web of connections, and our actions affect the entire system.
Our hormones exist in an ecosystem where everything hums and flows together, as a unit. It’s impossible to lay out explanations for their actions in a linear fashion.
Hormone stories flow like a Choose Your Own Adventure novel—a hallway with many doors that snake down long corridors and meet again, and interconnect.
Go through the door marked “estrogens”, and you encounter serotonin, cortisol, progesterone, insulin, thyroid hormones, leptin, BDNF, dopamine, norepinephrine, and many others.
Hormones are the conductors of your body’s personal orchestra, composed of thousands of musicians, a complex musical score, highly-trained arms, fingers, and mouths manipulating instruments: a million moving parts working together in harmony.
The best we can do to understand the entire interplay is to slow down the action, take a snapshot of it, and to try to understand why these symptoms are occurring in this individual.
Symptoms of Hormone Imbalances
Because hormones affect absolutely every system of our body, I am always attuned to the possibility of hormonal imbalances in my patients.
It helps to look at hormones in terms of their symptom patterns rather than how any one hormone affects us in particular.
Common signs of hormonal imbalance are:
- Fatigue, low libido, restless sleep, depression and anxiety, waking at 2 to 4 am, a high-stress lifestyle, and brain fog might indicate cortisol imbalance.
- PMS – and the more severe related condition, PMDD – infertility, fatigue and low libido, missed and irregular periods may be related to fluctuations in the hormones estrogen and progesterone, or low estrogen and progesterone levels. Many of these symptoms could also be related to estrogen dominance, in which estrogen is either high or normal, and progesterone is low.
- Endometriosis, a family or personal history of female cancers, anxiety and panic attacks, heavy and painful periods, frequent miscarriages, infertility, fibroids, fibrocystic breasts and weight gain around the hips and thighs can indicate estrogen dominance.
- High levels of male sex hormones like testosterone, irregular periods, weight gain, acne, and hair loss may indicate a female hormone condition called PCOS.
- Fatigue, brain fog, difficulty losing weight, puffiness, constipation, dry skin and hair, and low body temperature can be signs of hypothyroidism.
- Symptoms of reactive hypoglycemia, such as feeling dizzy, anxious and shaky between meals, sugar cravings, weight gain around the abdomen, difficulty losing weight, and low morning appetite, night-time carbohydrate cravings, and binge eating can all be related to insulin resistance and poor blood sugar control.
In my naturopathic practice, I see common patterns of symptoms that indicate certain hormonal imbalances.
These patterns often represent vicious cycles where our body is stressed beyond a capacity to balance these interconnected webs of chemical interactions, causing further imbalance.
Cortisol
Speaking of stories, here’s one I hear often.
You wake up in the morning, exhausted. Your brain is in a fog and you don’t feel alive until a cold shower or double espresso knock you out of your stupor.
Things get a bit better once you get moving, but you wonder why your energy never fully bounces back.
You used to play sports in university, you think to yourself. Now just thinking of sports makes you tired.
Is this what getting older feels like? You’re in your 30s.
The days at the office stretch on forever. Concentration and focus are difficult. You see a coworker whose name, you realize with horror, can’t be brought to mind.
You’ve known her for a year. Cynthia? Sylvia? Your brain hurts.
In the afternoon you think longingly of napping, but instead take your place in the long line for coffee and something carb-y like a cookie.
When it comes time for sleep you are either out like a light or find it hard to turn your mind off; you’re tired, as always, but also wired.
Sleep doesn’t feel restful, and you often wake up, sleepless, at 2-4am in the morning.
When your alarm rings a few hours later, the cycle begins again.
Cortisol, one of our stress hormones, has a circadian rhythm. Its levels are highest in the morning, about an hour after waking. Cortisol promotes energy, alertness and focus. It is also a potent anti-inflammatory hormone.
Cortisol is what makes us feel alive in the morning, bouncing out of bed like Shirley Temple and her curls.
Throughout the day our cortisol levels slowly dwindle (unless a major stressor causes them to spike abnormally). They are lowest in the evening, when melatonin, our sleep hormone begins to rise, inducing feelings of sleepiness, preparing us for a night of rest.
 Our modern day society, however, calls on cortisol to perform more than its fair share of work. Cortisol is around when we’re hauling ourselves out of bed after an inadequate night of rest.
Our modern day society, however, calls on cortisol to perform more than its fair share of work. Cortisol is around when we’re hauling ourselves out of bed after an inadequate night of rest.
Cortisol fuels gym workouts, gets us to our meetings on time, allows us to meet deadlines, tolerates traffic jams, responds kindly to tyrannical bosses, and makes sure the kids get to all their after-school events.
Cortisol is made in the adrenal glands, two endocrine glands located on each kidney, in response to signals from the brain that perceive stress in our environments and bodies.
When stress hormones levels are too high we experience a “tired and wired” feeling. During this time we might feel we thrive better under stress: workouts boost our energy, we have a hard time quieting down and we rarely feel hungry.
We might still struggle with weight gain, however, especially the abdomen and face, where cortisol tends to encourage fat deposition.
We might feel tension—tight muscles and shoulders, and body pain, as muscles clench up, preparing to fight or flee.
Chronic stress is associated with high levels of cortisol. We work long hours, late into the night. We go, go, go. This may give us a “high” or it may feel exhausting and depleting.
Many of us can exist in this state for months and even years. Sometimes a compounded stressor such as a divorce, accident, or loss, can tip us over the edge into a depleted, burnt out state.
Burnout, often following a period of prolonged stress, can be associated with low cortisol signalling. Our bodies have simply stopped being able to produce the stress hormones necessary to meet the needs of our daily lives, or glucocorticoid receptors in the brain and body cells, have stopped responding to cortisol.
Just as cell can be become resistant to insulin, they can also become resistant to cortisol. Too much (or even too little) of a hormone can cause cells to start ignoring their signalling, resulting in symptoms of low levels of the hormone in some areas of the body and high levels of the hormone in others.
Cortisol is a complicated molecule. It both encourages the stress response, but also turns it off, when levels reach a certain point.
Often, cortisol levels that are too low result in an impaired stress response, preventing our fight or flight system from properly shutting off—cortisol resistance can lead to further stress hormone disruption.
The result of an imbalance in cortisol, otherwise termed Hypothalamic Pituitary Adrenal (HPA) Axis dysregulation is weight gain, fatigue and brain fog, inflammation and immune system activation, digestive issues, restlessness, impaired sleep, decreased cognitive function, and mental health conditions, such as anxiety and depression.
When cortisol levels are low, the body makes adrenaline and noradrenaline to meet our needs, which often leads to anxiety and feeling shaky and nervous, contributing to symptoms of anxiety.
Cortisol also influences the function of our sex hormones, thyroid hormones, and our blood sugar. Imbalances in any of these other hormonal systems can be a result of an impaired HPA axis.
Cortisol Testing
The two main ways to assess the body’s levels of cortisol are through serum (blood tests) and saliva.
A study found both tests were equal when it came to diagnosing Cushing’s disease, a condition of highly elevated cortisol.
One of the advantages to salivary cortisol testing is the ability to obtain multiple samples in one day to be able to view a patient’s cortisol curve, in which cortisol peaks approximately one hour after waking and declines throughout the day.
The cortisol curve is measured by assessing 4 samples of salivary cortisol taken at 4 key points during the course of one day. It measures free cortisol, which may only represent about 5% of total cortisol in the body.
While salivary cortisol levels can be a good starting point for assessing the cortisol curve, it doesn’t tell us everything about the health of the glucocorticoid receptors or HPA system as a whole.
High cortisol levels may be seen in patients with low cortisol signalling, such as depression, anxiety and chronic fatigue. Errors in obtaining salivary cortisol samples (such as not taking samples at the right time) can lead to falsely low cortisol readings.
In my opinion, this makes symptoms and health history the most valuable tools for properly assessing HPA axis function.
Cortisol and Melatonin
Melatonin, our sleep hormone, also operates on a circadian rhythm. It is released by the pineal gland in the brain and induces sleep. Its release corresponds to a drop in cortisol levels at the end of the day.
That release is impeded by artificial light exposure at night, lack of daytime sun exposure, alcohol, stress, and HPA axis disruption, among other lifestyle and environmental factors.
Melatonin, like other hormones, can be tested for in blood, urine and saliva, but I find more value in assessing for sleep quality and quantity by taking a thorough health history while also restoring a patient’s sleep hygiene and HPA axis regulation.
Many patients with sleep issues can benefit from a trial of supplemental melatonin to see if that helps their sleep. Taking it 2 to 3 hours before bedtime to coincide with the body’s natural melatonin surge and taking a prolonged-release version to promote sleep maintenance are two strategies I use for helping patients sleep better.
Working on sleep and circadian rhythms is also beneficial for restoring HPA axis functioning.
The “Female” Hormones: Estrogen and Progesterone
The most prevalent female sex hormones are estrogen and progesterone. These two hormones eb and flow in distinct ways throughout a woman’s monthly cycle.
Estrogen creates an “M” shape, rising at the beginning of the cycle to its first peak around ovulation, half-way through the cycle. At this time women typically experience their best mood, energy, and motivation, perhaps noticing a rise in libido.
After ovulation, estrogen dips a little bit and then rises, peaking again about a week before a woman’s menstrual cycle is due.
After this, estrogen takes a nosedive, reaching low levels around the time that menstruation begins: Day 1 of the menstrual cycle.
Progesterone, on the other hand is largely absent the first half of the cycle, before ovulation. Then, it begins a steady climb to peak with estrogen, about a week before the arrival of the next period.
After peaking, just like estrogen, progesterone then takes a dip, which stimulates the uterine lining to shed, resulting in menstruation, in which the entire cycle begins again.
PMS and PMDD
My practice is populated by women who experience various forms of grief at different stages of their monthly cycles.
Many of my patients experience PMS, and the more severe PMDD (Premenstrual Dysphoric Disorder)—which is characterized by intense mood swings, irritability, depression, or anxiety, panic attacks and psychosis in the most severe cases— up to two weeks before their periods.
The mood changes in PMS and PMDD are associated with fluctuations in the hormones estrogen and progesterone, which can wreak havoc on our brain chemistry.
Estrogen has a beneficial effect on mood, increasing dopamine and serotonin action in the brain. Dopamine and serotonin are two antidepressant, feel-good neurotransmitters.
Estrogen also increases something called Brain-Derived Neurotrophic Factor (BDNF) a chemical that stimulates the growth of brain cells. This can boost memory, concentration, and cognition, as well as positively influence mood.
Progesterone breaks down into a chemical called allo-pregnenolone, which acts like GABA, a calming neurotransmitter, in the brain. Bioidentical progesterone therapy is often used as a treatment for anxiety and insomnia.
When estrogen and progesterone levels surge and drop suddenly, drastic fluctuations in mood can occur. Cravings for sweets, crying, lack of motivation, or severe anxiety can all occur when hormones drop right before a period is due.
However, elevated levels of estrogen can also be problematic. Estrogen stimulates dopamine, which typically makes us feel good, gives us energy, and helps to motivate us. In genetically vulnerable women, elevated levels of dopamine can cause excess irritability, low stress tolerance, and even mania or psychosis.
Estrogen also slows the recycling of the stress hormones epinephrine and norepinephrine, which can lead to symptoms of acute stress and anxiety, when dysregulated.
This means that dramatic rises and falls in estrogen throughout a woman’s cycle can cause her to feel irritable and anxious one week and unmotivated and depressed the other.
Smoothing out hormonal ups and downs can be a key factor in regulating a woman’s menstrual cycles and soothing her mood and emotions throughout the month.
Perimenopause and Menopause
Perimenopause is characterized by a declining production of the ovarian hormones estrogen and progesterone.
Estrogen levels tend to rise and fall dramatically throughout a woman’s remaining cycles, while progesterone levels tend to stay low.
The result of these changes are symptoms like hot flashes, night sweats, brain fog, fatigue, and depression when estrogen levels suddenly tank, and increased stress and anxiety when estrogen levels abruptly spike.
During this time, cycles may become irregular. Some of my patients comment that their periods are incredibly light one month and the heaviest of their lives another.
Some get periods every few months and some notice increased frequency, even spotting between cycles, or have a full-blown period every two weeks in more extreme cases.
Weight gain tends to drift from the thighs and buttocks to the abdomen. Once pear and hourglass-shaped figures begin to resemble apples.
Fatigue is a common symptom. Women may experience poor sleep due to night sweats from estrogen deficiency, and anxiety from insufficient progesterone.
What a joy, right?
Many of these perimenopausal symptoms are a relatively modern phenomenon, stemming from a dysregulated HPA axis.
After cessation of periods, it’s the job of the adrenal glands to take over sex hormone production. However, if the HPA system is preoccupied with organizing a stress response, this can affect the production of other hormones.
Impaired Estrogen Clearance
Many women struggle with symptoms that are related to relatively high levels of estrogen, often caused by impaired estrogen clearance.
These conditions include heavy and painful periods, fibrocystic breasts, or conditions like fibroids or endometriosis.
Chronically elevated estrogen levels also include a risk of certain hormone-associated cancers, such as breast cancer.
These women may experience irritability and anxiety through estrogen’s interaction with stress hormones, and also from a relative deficiency in progesterone.
A relatively high level of estrogens compared to progesterone is termed “Estrogen Dominance”.
 Estrogen is normally cleared through the digestive system: the liver and intestines.
Estrogen is normally cleared through the digestive system: the liver and intestines.
A sluggish and congested liver causing a slower rate of hormonal clearance (think of it like a clogged drain), an increase in environmental toxin exposure, or an overconsumption of alcohol, can slow the liver’s ability to regulate estrogen levels in the body.
Constipation and a dysbiotic gut can also impair estrogen clearance.
Symptoms of estrogen dominance include stubborn weight gain, typically around the hips and thighs, heavy and painful periods, tender and painful breasts, fibrocystic breasts, endometriosis, uterine fibroids, acne, cyclical mood swings, especially premenstrual anxiety and panic attacks, and irregular menstrual cycles.
Low Progesterone
Aside from impaired estrogen clearance, another pattern of estrogen dominance is low progesterone.
In this case, estrogen levels are normal or even low (as in the case of menopausal or perimenopausal women). However, an even lower progesterone level still results in a pattern of relative estrogen dominance.
This can cause some of the same symptoms as excess estrogen (anxiety, irritability, heavy and painful periods, weight gain, PMS, fibroids, fibrocystic breasts, etc.).
Low progesterone can also be a culprit in unexplained infertility or early term miscarriage, as progesterone maintains the uterine lining in pregnancy.
Progesterone is released from the ovaries after ovulation. Lack of ovulation, therefore, is a primary reason for low progesterone levels. Anovulatory cycles can occur in women with polycystic ovarian syndrome, women with high levels of physical and emotional stress, or women entering menopause.
Some progesterone, however, is also made in the adrenal glands, where it can be eventually turned into cortisol, aldosterone (a steroid hormone involved in salt-water balance in the body) and androstenedione (a male sex hormone), eventually making testosterone and estrogen.
Women with high cortisol demands due to chronic stress may shunt the progesterone made in their adrenal glands to producing other hormones that support the stress response.
Not only can stress alter ovulation and fertility through various other mechanisms, it can also rob the body of progesterone, directing any progesterone made towards cortisol production.
Testing Estrogen and Progesterone
Estrogen and progesterone can be tested reliably in saliva, blood and urine.
Month long salivary hormone testing of estrogen and progesterone can be an easy and effective way to track the eb and flow of these hormones throughout a women’s menstrual cycles.
In this test, women obtain a saliva sample every 3 to 5 days for the duration of the month to track how estrogen levels corresponds with progesterone and how both hormones rise and fall.
In my practice, however, I often start by running blood tests. I test hormones on day 21 (of a 28-day cycle) to coincide with progesterone’s peak. This can help us calculate the progesterone to estrogen ratio and establish whether the cause of estrogen dominance symptoms is high estrogen or low progesterone.
Blood tests offer the option of looking at estrone, which is a more problematic form of estrogen, as well as estradiol (the most common, metabolically active estrogen in the body). In blood we can also look at LH and FSH, two hormones produced in the brain and ovaries that orchestrate ovulation.
FSH tends to be high in women in menopause or perimenopause, while LH tends to be elevated in women with Polycystic Ovarian Syndrome (PCOS).
Dried urinary metabolite testing, or DUTCH, is an effective way to understand how hormones are broken down and processed by the body. Looking at the entire hormone breakdown pathway provides a more in-depth look at the complexity of hormones in a woman’s cycle, and can guide treatment in specific, useful ways.
The “Male” Hormones: Testosterone
Polycystic Ovarian Syndrome (PCOS) is one of the most common causes of infertility (and the most common endocrine disorder) in women of reproductive age. It affects about 10% of menstruating women.
PCOS is a collection of various symptoms and complex hormonal causes. However, it is characterized by missed periods, anovulation, male-pattern facial hair growth, especially on the upper lip, chin, breasts and abdomen, and the presence of cysts on the ovaries.
Other common symptoms of PCOS are weight gain, estrogen dominance, male-pattern hair loss (on the crown of the head), insulin resistance, infertility, and acne, especially hormonal cystic acne on the jawline.
PCOS is characterized by elevated levels of testosterone, a male sex hormone, or “androgen”, on blood work.
Acne, weight gain, infertility, and hair loss are the main symptoms that bring women with PCOS into my office.
PCOS is a complex process that involves an overproduction of testosterone in the ovaries coupled with insulin resistance. Therefore, balancing blood sugar through diet and lifestyle can have a major impact on symptoms.
The conventional treatment for missed or absent periods is oral contraceptives, which of course doesn’t treat the underlying cause of anovulation. That’s why women with PCOS often seek naturopathic and functional medical solutions to treat the root cause.
Testing for PCOS
When I meet a new patient with PCOS, I often test her blood for estradiol and progesterone levels at Day 21 of her cycle. A very low progesterone level may indicate that she has not ovulated that cycle.
We also test LH and FSH. A high LH:FSH ratio can be indicative of PCOS even if cysts are not present on an ovarian ultrasound.
Other important tests that are often ordered are free testosterone and DHEA-S, another male hormone made in the adrenal glands.
Glucose control and insulin resistance can be assessed by looking at fasting blood glucose, fasting insulin and HbA1c (a marker that looks at long-term glucose control).
Prolactin, another hormone released by the pituitary gland, can sometimes be elevated in anovulatory women with PCOS.
A 4-point salivary cortisol test may be useful in women with PCOS who are also experiencing symptoms of cortisol dysregulation, which can contribute to insulin resistance and affect ovulation and hormone regulation, particularly progesterone production.
Prolactin
Prolactin is a hormone released by the pituitary gland to promote milk production after child birth.
However, some women will have elevated levels of prolactin in blood, despite not currently pregnant or breastfeeding.
Called hyperprolactinemia, elevated prolactin may be a cause of anovulation, mimicking some symptoms of PCOS and menopause, including hot flashes, absent or irregular periods, infertility and even milk discharge from the breasts.
Hyperprolactinemia may be caused by low calorie diets, liver issues, hypothyroidism, and issues with the pituitary gland itself.
Prolactin can be tested in blood. If levels are elevated, an MRI must be conducted to rule out a physical issue with the pituitary gland, such as a tumour.
Oxytocin
Oxytocin is a hormone produced in the brain and secreted by the pituitary. It aids in childbirth. Also termed the “love hormone,” it’s associated with feelings of intimacy and connection.
While high and low levels of blood oxytocin can be possible in men and women who are not pregnant or breastfeeding, the clinical applications of it are not fully known.
Thyroid Hormones
The thyroid, a butterfly-shaped gland on our neck, is the master thermostat of the body, controlling heat and metabolism. It pumps out thyroid hormones T4 and T3, which tell cells to burn fuel, creating energy and heat.
Because our thyroid hormones interact with the cells in every body system, symptoms of hypothyroidism, or low thyroid function, can be incredibly diverse.
Common symptoms of hypothyroidism are weight gain or inability to lose weight, fatigue and sluggishness, brain fog, hair loss, low body temperature, constipation, dry skin and hair, puffiness, infertility, and altered menstrual cycles, such as missed periods or heavy periods.
Aside from autoimmunity, other causes of low thyroid function can be HPA axis dysregulation and chronic stress, a very low calorie or very low carbohydrate diet, sudden weight loss, a deficiency in nutrients needed for thyroid function such as iron, zinc, iodine and selenium, and a body burden of environmental toxins such as heavy metals.
Testing Thyroid
To assess thyroid function, conventional doctors will test a hormone called Thyroid Stimulating Hormone, or TSH. TSH is not a thyroid hormone, but a hormone made in the brain that urges the thyroid to pump out the thyroid hormones T3 and T4. It gives doctors an indirect measure of thyroid regulation.
When TSH levels are high, this suggests that thyroid function is sluggish; the brain needs to send a louder signal to get an unresponsive thyroid to work.
However, TSH is only a periphery marker of total thyroid function, not giving us the whole picture. Also, TSH ranges on conventional lab tests may fail to pick up some cases of subclinical hypothyroidism or impending cases of autoimmune thyroid conditions, otherwise termed Hashimoto’s Thyroiditis, which is the most common cause of hypothyroidism.
To properly assess thyroid function in someone with symptoms of thyroid dysfunction, a slightly elevated TSH, or a family history of Hashimoto’s, I will order a thyroid panel: a blood test measuring TSH as well free thyroid hormone (T3 and T4) levels.
It’s also important to assess for autoimmune thyroid conditions by testing for anti-thyroglobulin and anti-thyroperoxidase antibodies. Both of these antibodies, when elevated, suggest the presence of an autoimmune thyroid condition.
Insulin
Some of the most common hormonal dysfunctions I see in my practice are insulin resistance and reactive hypoglycemia: blood sugar imbalance.
These issues often lie at the heart of other hormonal imbalance patterns, such as irregular menstrual cycles or HPA axis dysregulation.
When we eat, glucose enters our bloodstream, providing fuel for our cells. Insulin helps our cells access this hormone, spiking with each meal.
The higher the meal is on the glycemic index (i.e. the more sugar or refined carbohydrate it contains), the higher our post-meal blood sugar and insulin spikes will be.
Without insulin, we would slowly lose energy and die, unable to get precious glucose into our cells. Individuals with type I diabetes cannot make insulin. They must inject it daily to keep their cells fuelled and blood sugar stable.
For the rest of us who do make insulin, large blood sugar spikes after a meal can be problematic.
Insulin is a storage hormone. It helps energy get into cells, and it helps build muscle and brain cells, but it also blocks the breakdown of fat cells, blocking weight loss.
Insulin also drives down blood sugar levels. When blood sugar rises too quickly after a meal, a large insulin response can drop blood sugar levels too drastically, causing reactive hypoglycemia, or feeling “hangry” (hungry, angry, irritable, tired, light-headed, weak and dizzy) in between meals.
Individuals who experience hypoglycemia feel irritable, shaky, dizzy and anxious between meals. They often suffer from anxiety and panic attacks, and feel hungrier at night.
They may wake up in the middle of the night, as their bodies are unable to go 8 hours (the length of a decent night’s sleep) without food. This causes them to wake up, restless and perhaps anxious, in the early hours of the morning.
These individuals, paradoxically, rarely feel hungry at breakfast time.
I often see anxious patients wake from a restless sleep and toss back only a coffee in the morning, skipping breakfast due to slight morning nausea.
At 10 am, feeling ravenous and shaky, they might scarf down a high-glycemic bagel or croissant. Later on, they’ll enjoy a light lunch—maybe a sandwich—often feeling foggy and lightheaded after eating it.
At 2 to 4 pm, they may feel like an afternoon nap, instead indulging in a coffee and sweet treat to buy them some energy for the remaining hours of the work day.
Finally, after enjoying a larger dinner once they get home, they find themselves snacking all night long. Their bodies are finally urging them to ingest the nutrients they were lacking throughout the day.
They then fall into bed, feeling full, restless and wired, and the cycle begins again.
When our blood sugar falls, we not only feel hangry, weak, and crave processed carbs, our HPA axis also gets stimulated.
Cortisol, a glucocorticoid, can help our body control blood sugar, bringing it into the normal range after insulin sends it tanking too low.
This drop in blood sugar, therefore, needlessly triggers a stress response from the adrenal glands, which can further worsen anxiety, HPA axis dysregulation, and glucocorticoid resistance.
When blood sugar and insulin are spiked repeatedly for days, months, and years on end, cells stop responding attentively to insulin’s signal. Like our response to a pesky telemarketer, cells eventually stop picking up the phone when insulin calls.
However, cells still need insulin. More and more insulin must be released to trigger the same response from insulin resistant cells. This makes cells even more resistant, as they require even more insulin release the next time blood sugar rises to get glucose into the cell for fuel. And so the cycle becomes vicious.
Elevated insulin levels cause inflammation, fat gain, fatigue, depression, reactive hypoglycemia, and HPA axis dysregulation. The more resistant our cells become to insulin, the more cortisol must be called on to maintain blood sugar levels.
PCOS is also characterized by higher insulin levels. This prevents ovulation, causing infertility and female hormone imbalance.
When insulin resistance persists, type II diabetes, where the body is no longer able to keep blood sugar in a safe range, develops.
Type II diabetes is characterized by chronically high blood sugar—which poses a danger to small blood vessels, and is a potent inflammatory condition, increasing the risk of heart disease—and elevated insulin.
It affects almost 10% of the adult population and is the 7th leading underlying cause of death in North America, costing 350 billion dollars a year to manage in the United States alone.
Insulin-related weight gain can affect female hormones, as fat cells make estrogen in the body, leading to estrogen dominance.
Insulin also interacts with a hormone called leptin, which is created by fat cells in response to calorie intake. When body fat levels get too high, cells can become leptin resistant. The body no longer senses dietary calorie intake, leading to increased hunger. This exacerbates the problem of weight gain and insulin resistance.
Testing for Insulin Resistance
When I meet a patient who is presenting with stubborn weight gain, estrogen dominance and stress, I assess their blood for insulin resistance by looking at blood levels of fasting insulin and fasting glucose.
With these two values a calculation that measures insulin resistance, called the HOMA-IR, can be performed. This can give us a baseline measure of how well the body is compensating to control blood glucose.
I also run HbA1c, which looks at glucose levels over 3 months. I will often run a blood cholesterol panel, and inflammatory markers, such as CRP.
Insulin resistance often puts all of our hormones on a rollercoaster, which becomes very difficult to get off of unless we prioritize the diet and lifestyle interventions that address blood sugar control.
Assessing Hormones
When presented with a patient suffering from a complicated symptom pattern, I begin by taking a thorough health history in which we investigate:
- Energy levels,
- Sleep quantity and quality,
- Mood and mental health history,
- Period health history,
- Family history,
- Dietary intake and exercise,
- Health risk factors like smoking, alcohol use, and past health history.
Depending on how clear the patient’s symptom picture presents, we may opt to make some changes before testing, to gauge their body’s response to an increase in nutrient intake.
Then, if necessary, I will order a comprehensive blood work.
Blood testing might include a thyroid hormone panel, and an in-depth look at female hormones, fasting insulin and fasting blood glucose, and other markers that help us assess health, such as cholesterol and inflammatory markers, or nutrient levels.
Patients requiring a more comprehensive view of their cycles may opt for month-long salivary testing. Others may opt for a dried urine test that looks at hormonal breakdown in the body.
A Sample Case
Jenny (name changed for privacy) came to me feeling fatigued and anxious.
She had suffered from anxiety periodically as a teen, but now at age 46 she was experiencing bimonthly panic attacks that seemed to occur cyclically; the panic would come around ovulation and premenstrually.
It was hard to tell, however, because Jenny also claimed that her periods were “all over the place”. One month they were heavy and painful, causing her to take time off work, crouched on the bathroom floor in agony. Other months she barely noticed them, experiencing some light spotting, if anything at all.
Very troubling to her was her major mood volatility, which she described like a “switch” that would suddenly flip on or off, causing her to breakdown at work or pick fights with her family.
Then, almost as suddenly, the cloud would lift and she would be her cheerful, friendly, loving self again.
It was maddening, both to her and those living with her during these darks times, she said.
She also noticed disrupted sleep and weight gain around the abdomen, which seemed to ignore her intense workouts and strict dietary regime.
Jenny was highly accomplished at her high-pressure job and commented that she thrived on being busy and achievement oriented.
I tested Jenny’s blood estradiol, estrone, progesterone, LH, and FSH levels one week before her next expected period, had her fill out a weekly diet diary, and gave her some recommendations about sleep and supplement intake.
Jenny’s blood revealed elevated FSH, indicative of impending menopause (FSH encourages the ovaries to ovulate, as TSH encourages the thyroid gland to make thyroid hormone). She also had low estradiol, and low progesterone, but elevated levels of estrone, the more problematic of the estrogens.
According to her labs and history, Jenny was experiencing estrogen dominance and perimenopause. Many of her symptoms were stemming from elevated estrone, low progesterone and a disrupted HPA axis.
Together, we worked on her diet to provide her body with the nutrients needed to make hormones and to support her brain, mood and adrenal glands.
We used herbs and dietary nutrients to promote liver estrogen clearance and to support Jenny’s adrenal glands.
We addressed the stress in her life, encouraged relaxation, and made sure her body was supported in its ability to make and respond to cortisol.
After a few months, Jenny reported a reduction in hot flashes, better sleep and feeling calmer. She had a reduction in her waist line and better energy and mood.
Our hormones, when imbalanced, can cause vicious cycles in the body that trap us in a state of worsening imbalance.
Through correctly assessing these common hormonal patterns through a health history and appropriate testing, and then making diet, lifestyle and supplement suggestions addressed at stopping these cycles, naturopathic doctors can address underlying hormonal issues that might be causing these complex and troublesome patterns of hormone disruption.

by Dr. Talia Marcheggiani, ND | Apr 5, 2018 | Anxiety, Depression, Detoxification, Digestion, Emotional Wellness, Emotions, Endocrinology, Estrogen Dominance, Fertility, Gut Microbiome, Hormones, Mental Health, Nutrition, Self-care, Stress, Women's health
 Since publising the original article about the Mirena IUD on this blog, thousands of women have come out of the woodwork writing to me asking for help.
Since publising the original article about the Mirena IUD on this blog, thousands of women have come out of the woodwork writing to me asking for help.
When I originally wrote the article, I was spurned on by my observations of the women in my practice who had experienced a rise in estrogen dominance and low progesterone after the insertion of their IUDs (which were often inserted to treat hormone imbalances!).
At that point I never imagined that so many women would be affected by the IUD, or that even more were suffering from so many hormonal symptoms that drastically affected their lives and health.
It makes sense: our society does not set us up for proper hormonal function.
Our diets are carbohydrate-heavy, promoting insulin resistance and blood sugar dysregulation, which impacts our ovaries’ ability to make estrogen properly.
An excess amount of body fat produces more estrogen in the body and acts as a reservoir for the toxic estrogens in our environment.
We lack many of the micronutrients necessary to process our hormones properly, such as vitamin D, B vitamins, magnesium, zinc, omega 3 fatty acids, glutathione, and amino acids.
Many of us have impaired or suboptimal liver function, or sluggish digestion, which keeps hormones in our bodies around longer than they should be.
A dysbiotic gut has the tendency to turn estrogen in the gut back “on”, putting it back into circulation when it was otherwise on its way out of the body.
Stress alters our hormonal function, including our ability to make progesterone, DHEA-S, convert thyroid hormones, and process estrogen properly.
Xenoestrogens in our food and environment, from plastics, fragrances, pesticides, and processed soy products, contribute to overall body burden of the hormones in our body, throwing off our delicate balance, and contributing to symptoms.
The result of all this is that many women suffer from hormonal imbalances.
10% of women have some form of PCOS, or Polycystic Ovarian Syndrome, characterized by the body’s inability to properly make progesterone or estrogen, instead making loads of male hormones, like testosterone. PCOS alters fertility, promotes weight gain, and causes things like unwanted facial hair growth, acne, and missed periods. PCOS is often connected to stress and insulin resistance.
Many women in my practice suffer from PMS or PMDD, experiencing often debilitating symptoms sometimes even two weeks before their periods begin. They might get migraines, intense cravings for sugar, and massive mood changes, such as anxiety, intense irritability, or devastating depression. Panic attacks can occur at this time as well. Many of them comment that their mood and personalities flip once their hormones levels reach a certain point, causing them to act like different people. This can jeopardize their relationships with spouses and children, coworkers, friends and family.
Tender and painful breasts, or breast lumps, are also common in many of these women.
Acne, weight gain, stress, fatigue, disrupted sleep, depression and anxiety are all symptoms I see in women with hormonal imbalances.
Many women have horrific cycles, experiencing painful and heavy periods that often cause them to miss days of work every month. Many of these women struggle to keep their iron levels in the optimal range, suffering from hair loss, fatigue and weakness.
Many women are diagnosed with fibroids, or endometriosis, or are concerned about their risk of female cancers like breast, ovarian, uterine and cervical cancer.
All of these symptoms are often linked to relatively higher levels of estrogens compared to progesterone, sometimes termed Estrogen Dominance by functional medical practitioners who look at the underlying causes of bodily imbalances.
I feel terrible that I can’t help more of the women who write to me. My license prevents me from giving advice to those who live abroad, especially to non-patients over the internet. It’s a shame, however, because oftentimes the solutions are relatively simple, despite how complicated many of these symptoms might seem.
I’m hoping that this article can provide some direction to many of the women who suffer.
Firstly, I want to state that I am not against birth control or even the Mirena IUD (or other IUDs, for that matter). The vast majority of women with the IUD tolerate it. For many women with debilitating heavy periods and endometriosis it can be the only viable solution that makes life tolerable.
In my social practice at Evergreen, many of the women I see experiencing homelessness, drug addiction, or PTSD from relationship trauma, rely on the efficacy of IUDs to prevent unwanted pregnancies. Their lives often don’t allow for them to remember to consistently take pills every month.
Many women don’t tolerate combination birth control because of a history of blood clots, female cancers, or migraine headaches associated with their periods, and therefore the Mirena IUD, which is progesterone only, is a safe alternative for preventing unwanted pregnancy.
That all being said, many women do suffer on the Mirena IUD (or other forms of birth control). They were perhaps put on the Mirena to deal with some of the above symptoms of hormonal imbalance, or for contraception. Many of them noticed that their symptoms became worse after insertion of the IUD.
How the Mirena IUD and Birth Control Works:
The Mirena works by secreting small amounts of progestins, a synthetic form of progesterone, into the uterus and surrounding tissues. While it is not fully known how the Mirena works, the end result is a suppression of ovulation. This results in either very light periods or a complete cessation of periods until the IUD is removed (after 5 years when its hormones run out).
It is important to say here that, while birth control can certainly treat the symptoms of hormonal imbalances, it does not correct them.
All forms of birth control, with their synthetic versions of the hormones estrogen and progesterone, simply induce further hormone imbalances in the body. They introduce versions of hormones that may suppress or alter symptoms (such as heavy and painful bleeding, or acne), but the versions of hormones are not fully recognized by the body and therefore don’t fully replace all the hormones’ important functions, such as mood regulation, immunity, or blood sugar balance.
The effects of both altering the body’s natural hormonal balance, while ignoring the underlying cause of hormonal issues, is often what causes symptoms to continue or worsen.
For example, women with PCOS are prescribed birth control to manage acne or promote monthly periods. However, when women with PCOS miss periods, it is because they are not ovulating. The missed periods are not the problem; the lack of ovulation is.
Despite that, many women with PCOS experiencing amenorrhea (or missed cycles) will be prescribed birth control. However, birth control does not address the underlying cause of amenorrhea. It simply further suppresses ovulation (because its main purpose is to prevent unwanted pregnancy).
The periods you get while on birth control are not periods. Periods from birth control are withdrawal bleeds. After 21 days of taking hormonal pills, pills are stopped or replaced with placebo pills. The withdrawal of hormones in the pills induces a bleed that resembles a period, but is not one.
Hormonal contraception does not correct hormonal imbalance, it imposes further hormonal imbalance to manage symptoms. This is not always bad!
But it is an important difference.
Many women do require symptom suppression, particularly if their symptoms are severe. Many individuals in my practice experience periods so heavy that the only way for them to get through the month is with an IUD. Genetic variability in how our bodies process hormones can make us susceptible to intense hormonal symptoms, through no fault of our own.
In my opinion, however, it is important to attempt to address the underlying cause and to set our bodies up for better hormonal regulation, making as many changes as our lifestyles will allow.
What You Can Do About It:
 If you are like any of the people I described above who seek my help, there are a few things that you can do to get started on correcting hormones.
If you are like any of the people I described above who seek my help, there are a few things that you can do to get started on correcting hormones.
Working With a Professional:
The first thing I advise is finding a licensed naturopathic doctor or functional medicine practitioner who understands hormones, can order lab tests, and will address the underlying cause of your hormonal imbalances by taking the time to fully understand your body and lifestyle.
This practitioner might be a naturopathic doctor (you can find one in North America by looking one up at naturopathic.org), or a medical doctor, a chiropractor, or a highly skilled nutritionist or nurse practitioner. Research this person well, read their articles, and perhaps book in with them for a complimentary meet and greet.
Testing:
I often test patients using simple blood tests, on day 21 of their cycles (or about 7-9 days before they expect their next period).
I will test their blood, looking for anemia, will test iron and B12 levels, homocysteine (to gauge their ability to methylate), vitamin D, cholesterol (to see if their diets are promoting proper hormone synthesis), estradiol, estrone (the more toxic, problematic estrogen), progesterone, free testosterone, a thyroid panel, fasting glucose and fasting insulin (to calculate insulin resistance using something called the HOMA-IR), HbA1C (to look a long-term blood glucose control), FSH and LH (two hormones made in the brain that talk to the ovaries and orchestrate the menstrual cycle), DHEA-S, to name a few.
Some women will require more testing. Others will require less.
These labs are interpreted from a functional perspective. Even though you are in the “normal” ranges (which take into account the entire population, many of which are not healthy—they are seeing their doctors, after all!), these blood markers may not be optimally balanced, giving us an opportunity to correct things before they go further.
Testing allows us to match symptoms to underlying imbalances and to be able to properly direct treatment protocols. Women with estrogen dominance may be experiencing high levels of estrogen and normal progesterone, which indicates a body burden of estrogen or impaired liver and digestive system clearance. Other women may be experiencing normal levels of estrogen but low progesterone, indicating a failure of their bodies to ovulate, due to high stress, and PCOS (or the Mirena IUD and birth control pill).
Other options for hormonal testing are month-long salivary hormone testing, or DUTCH testing, which looks at hormone breakdown in the urine. I sometimes run these tests, but find that blood testing is useful, accurate, and more cost-effective.
Treatment:
 Once you understand your individual hormonal situation through testing (and through working with a practitioner who is putting the testing together with your symptoms and health history), your practitioner may recommend a variety of treatments.
Once you understand your individual hormonal situation through testing (and through working with a practitioner who is putting the testing together with your symptoms and health history), your practitioner may recommend a variety of treatments.
I personally combine diet and lifestyle with key herbal and nutritional supplements, to target what is going on under the surface with my particular patients.
These treatments may include herbs that boost ovulation, aid liver detoxification, or regulate the stress response. I might recommend nutraceuticals that encourage methylation, or aid in hormone production.
My treatments take into account the individual’s symptoms, labs, diet, lifestyle, and any other health issues she may be facing like fatigue, digestive disturbances, or poor sleep.
What You Can Do Today:
Barring more individualized assessment and advice, there are some best lifestyle practices that can help most women balance their hormones better, whether they are still using birth control to control and address their hormonal symptoms or prevent pregnancy.
Diet:
When it comes to diet and hormone support, we need to ensure that we are balancing blood sugar, boosting liver detoxification pathways, promoting hormone synthesis, and supporting digestion, especially if experiencing constipation.
- Consume more leafy greens: kale, spinach, collards, beet greens, arugula, etc. Eat 1-2 cups of these foods every day. Leafy greens contain active folate, which boosts methylation and detoxification. They also contain magnesium which is essential for hormonal regulation as well as 300 other important biochemical reactions in the body that balance mood and hormones.
- Consume more cruciferous vegetables: broccoli, cauliflower, brussel sprouts, cabbage, bok choy, etc. Eat 1-2 cups of these foods every day. Crucifates help the body make glutathione, and contain indole-3-carbinole, which helps eliminate excess estrogens from the body. Broccoli sprouts are potent players in these pathways. Consume them as often as possible.
- Ensure adequate dietary fibre intake: I often recommend ground flaxseeds or chia seeds in smoothies, avocados, fruits and vegetables and legumes (if tolerated) to make sure that women are having regular bowel movements to clear excess estrogens out of the body. 2 tbs of ground flaxseed (or more) every day can help balance estrogen levels and promote daily bowel movements.
- Balance blood sugar: consume protein, fat and fibre at every meal. Avoid refined starches and flours. Avoid all sugar, even natural sugar like maple syrup, coconut sugar, cane sugar, honey, agave, etc. Try stevia or avoid sweets. Limit carbs (grains, legumes, root vegetables like potatoes or sweet potatoes, to 1/2 cup to 1 cup per meal). Only consume whole grains like quinoa, buckwheat, steel cut oats, millet, and teff. Cook them yourself!
- Avoid soy, particularly processed soy, like vegan burgers, or soy milk.
- Consume omega 3 fatty acids in fatty fish like salmon and sardines, or nuts and seeds like flax and chia seeds, walnuts, and pumpkin seeds. Get 2-4 tablespoons of these nuts and seeds every day and 3-4 servings of fatty fish a week.
- Consume animal products: eggs contain choline, which is essential for liver function, meat contains vitamins B6 and B12, which are essential for hormonal regulation and production. Cholesterol in animal products are the backbones of our sex hormones. Iodine, found in animal foods, regulates estrogen balance in the body. If possible, try to obtain organic animal products from pastured or free-range animals to boost omega 3 intake, to lower your impact on the environment, and to promote animal welfare.
Other Lifestyle Practices:
Boost progesterone production by managing stress:
- Establish a self-care routine: plan regular vacations, even small outings, do meditation or yoga, take breaks from work, spend quality time with family, have a plan to get your work done on time, ask for help.
- Sleep! Aim for at least 8 hours of sleep, and try to get to bed before 12am. Practice good sleep hygiene by avoiding electronics before bed, keeping the bedroom as dark as possible, and setting a bedtime and wake time, even on weekends. Body scan meditations and some key supplements can be helpful for resetting circadian rhythms. Regulating blood sugar can have a major impact on improving sleep. Talk to your functional medicine doctor or naturopathic doctor for individualized sleep solutions.
Eliminate exposure to toxic estrogens and boost estrogen clearance:
- Avoid exposure to xenoestrogens: whenever possible use natural body products, deodorants and shampoos, or “edible” body products for face and hair. Avoid plastic water bottles and plastic food containers. Use natural cleaning products around the house. Avoid fragrances and processed foods, especially processed soy.
- Encourage sweating: get regular exercise or engage in regular sauna therapy. If you don’t have access to a sauna, epsom salt baths can also work—anything that helps you sweat. Heat therapy has also been shown to benefit mood and the stress response.
- Heal your digestion: make this a priority with your naturopathic doctor, so that you can absorb the nutrients from the foods you’re eating as well as encourage daily bowel movements and optimal microbiome balance.
- Maintain a healthy weight: body fat is metabolically active and can increase overall estrogenic load. Work with your naturopathic doctor to manage your weight. We often attempt to lose weight to become healthy, however I find my patients have far more success (and fun!) getting healthy in order to lose weight. Healthy weight loss often involves managing stress, sleeping 8 hours a night, avoiding sugar and processed foods, and regulating blood sugar, as well as encouraging proper sweating and liver detoxification.
Want to balance your hormones, energy and mood naturally? Check out my 6-week foundational membership program Good Mood Foundations. taliand.com/good-mood-learn

by Dr. Talia Marcheggiani, ND | Nov 3, 2017 | Anxiety, Autoimmune, Detoxification, Diet, Endocrinology, Estrogen Dominance, Fertility, Genetics, Hormones, Mental Health, Nutrition, Vitamins
 Is your multivitamin or B-complex making you sick?
Is your multivitamin or B-complex making you sick?
Take a look at the label on your multivitamin or B-complex and see if it contains “folic acid”.
Folic acid is often used interchangeably with “folate”, which is a vitamin needed for DNA synthesis and repair.
Every time our bodies make new cells (which is all the time), we need folate to move that process along.
Because very few of us North Americans get enough folate from leafy greens, folic acid, a synthetic precursor to folate, has been added to grain products, to “fortify” them.
Folate deficiency in pregnant women can lead to neural tube defects. Therefore making sure that your body has enough folate, especially if you’re pregnant or planning to conceive, is essential.
However, folic acid, the synthetic vitamin is NOT the same as the folate (look at the bottom of the chart below, another word for folate is 5-methyltetrahydrafolate, or 5-MTHF) that our bodies use for cell division and DNA synthesis.
As you can see by the picture, folic acid needs to go through several stages of transformation before it can be of any use to the body.
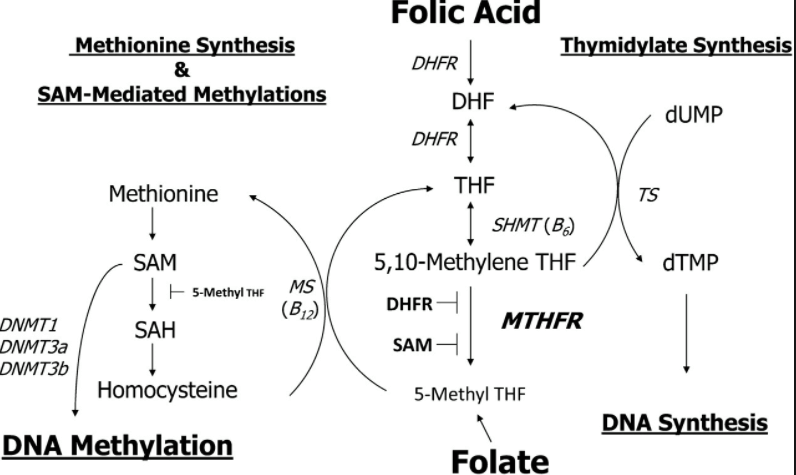
All of us are really poor at converting folic acid to DHF (first step in the pathway). This step is faster in rats. In humans, it’s abysmally slow.
This means we take folic acid from supplements and fortified grains and slowly pass it through the narrow DHFR sieve that all of us are born with. This slowly transforms our synthetic folic acid into DHF.
The same DHFR enzyme must take DHF and turn it into THF. Two steps: folic acid –> DHF –> THF. So far, none of these products is useful.
3 steps and 2 enzymes later, our body makes a product called 5,10 methylene THF, or folinic acid, which can be used for DNA repair and synthesis.
After that, an enzyme called MTHFR turns folinic acid into folate (5-MTHF). And yes, MTHFR does remind you of the word you’re thinking of!
About 40-60% of us are poor at the last step, making 5-MTHF, which results from a slow or completely impaired MTHFR gene which has trouble producing a fully functioning MTHFR enzyme.
Slow enzymes mean very few of us are going to take the folic acid from foods and cheap vitamins, and turn them into methylfolate.
Methylfolate (remember, NOT folic acid), is needed for important chemical reactions called “methylation” reactions.
Methylation is needed for with detoxification, liver function, managing inflammation, hormone production and recycling, and producing neurotransmitters. Research is establishing a connection between MTHFR gene mutations and mental health conditions, autoimmune conditions and heart disease, among other common health complaints.
Folic acid, when added to supplements isn’t just useless, however.
When it can’t be broken down (and remember, all of us are slow at the first stop, some of us just plain can’t perform the last step), it builds up in tissues, and can block ACTUAL methylfolate action.
It can also trigger inflammatory reactions.
Not good.
Most multivitamin and B complex brands at health food stores contain cheaper forms of B vitamins. Companies use folic acid and a cheaper, synthetic form of B12, called cyanocoblamin, when making products to cut costs.
This doesn’t mean you have to shell out a lot of cash for quality B complex vitamins, it just means you need to be smart about the B-complexes you buy.
B-complex vitamins can be useful for those who experience inflammation, hormone imbalances and chronic stress. We tend to use more B-vitamins, which are water-soluble, when stressed, and when on certain medications, such as birth control pills. Supplementing in these cases can be extremely helpful for boosting energy and mood, while lowering symptoms of PMS and inflammation, among other things.
Most of the patients who come into my office already on a B complex are on a form that contains folic acid. At best, their body is working harder than needed to convert this synthetic vitamin into something useful. At worst, this product may be causing them harm.
The first thing you can do, is check your multivitamins and B-complex products and see if they contain “folic acid” or “cyanocobalamin”. If so, you can toss them.
You can also consider getting tested to see if you have an MTHFR mutation. Keep in mind that naturopathic doctors who are registered in Ontario, Canada cannot recommend or interpret genetic testing.
Next, you can reassess your diet. Folic acid is also added to enriched grains. Those who are particularly sensitive to folic acid, may experience a worsening of inflammatory symptoms and mental health issues when consuming high amounts of these foods.
Also, eat plenty of leafy green vegetables, which DO provide your body with a useable form of folate, among their many other health benefits.
Finally, if you’re considering getting pregnant, have a naturopathic doctor assess your prenatal vitamins to tell you if the form of folate you’re taking is appropriate for you.